The Most Important Things to Know About Type 1 Diabetes


What is type 1 diabetes?
Like all types of diabetes, type 1 diabetes (T1D) manifests as high blood sugar. But its development is totally unique, caused by an autoimmune condition, a disorder where the immune system mistakes a part of your own body as an enemy.
In the case of type 1 diabetes, that enemy is the pancreas. “The immune system destroys the beta cells in the pancreas because it sees them as foreign,” says Jane Reusch, M.D., a professor of medicine, bioengineering, and biochemistry and the associate director of the Ludeman Family Center for Women’s Health Research at the University of Colorado, in Aurora.
This means the pancreas doesn’t produce (or makes very little) insulin—a hormone that helps blood sugar (glucose) get into cells throughout the body, so it can be used for energy. Without the insulin, blood sugar rises; this can lead to a variety of serious complications if not treated properly.
What causes type 1 diabetes?
So it’s an autoimmune condition. But like all autoimmune conditions, the underlying mechanism is a bit hazy. Experts still don’t know why the immune system—the system in the body that protects us from infection and fights off viruses and bacteria—turns on the pancreas in those with T1D. Here’s what they do know about its causes.
Risk factors for type 1 diabetes
- Family history: There’s a strong genetic component at play. Those with no family history of the disease have a 0.4% risk of developing it, while having a parent with the condition raises that to 5%. The risk goes up even more, to somewhere between 10% and 25%, if both parents have type 1 diabetes.
- Virus exposure: Having certain viruses—such as congenital rubella, Coxsackievirus B, cytomegalovirus, adenovirus, and mumps—in utero or early childhood is thought to play a role. “It has long been suspected that a viral infection may trigger type 1 diabetes,” says Dr. Tom Donner, M.D., an associate professor of medicine and the director of the Johns Hopkins Diabetes Center, in Baltimore. “Though this remains to be proven.” One theory is that when your immune system jumps into action to fight a virus, it goes into overdrive, ultimately attacking the healthy cells in the pancreas.
- Cold climates: Type 1 diabetes tends to develop more often in winter than summer and is more common in places with cold weather. Again, researchers aren’t sure why, but it may have something to do with higher rates of vitamin D deficiency in those regions.
- Pancreas injury: If the pancreas is damaged—due to an injury or a condition like pancreatitis—this ups the risk of triggering T1D.
What are the symptoms of type 1 diabetes?
The signs of T1D can appear suddenly and be severe. Knowing the symptoms to look for and alerting your doctor as soon as possible can help you avoid the more serious complications. In children, the most common symptoms—urinating frequently, drinking large quantities, losing weight, and becoming more and more tired—are fairly prominent. Adults can also experience all of the above, but the other symptoms can be easier to overlook, including blurred vision, slow-healing cuts and sores, and vaginal yeast infections.
How is type 1 diabetes diagnosed?
Your doctor will perform a simple blood test to see if you have type 1 diabetes (and likely repeat it to make sure a positive result was accurate). Results that indicate you have type 1 diabetes include:
- A fasting blood glucose level higher than 126 mg/dl (milligrams per deciliter)
- A random blood glucose level higher than 200 mg/dl
- Elevated blood glucose on an oral glucose tolerance test higher than 200 mg/dl
- An A1C level greater than 6.5%
Doctors can often determine that it’s type 1 as opposed to type 2 by looking at other health issues. Having a high BMI (body mass index), blood pressure, or cholesterol is more common with type 2, while having another autoimmune disease is more common with type 1. Additional tests can also be used to look for specific autoantibodies in the blood or ketones (a waste product) in the urine that occur only with type 1.
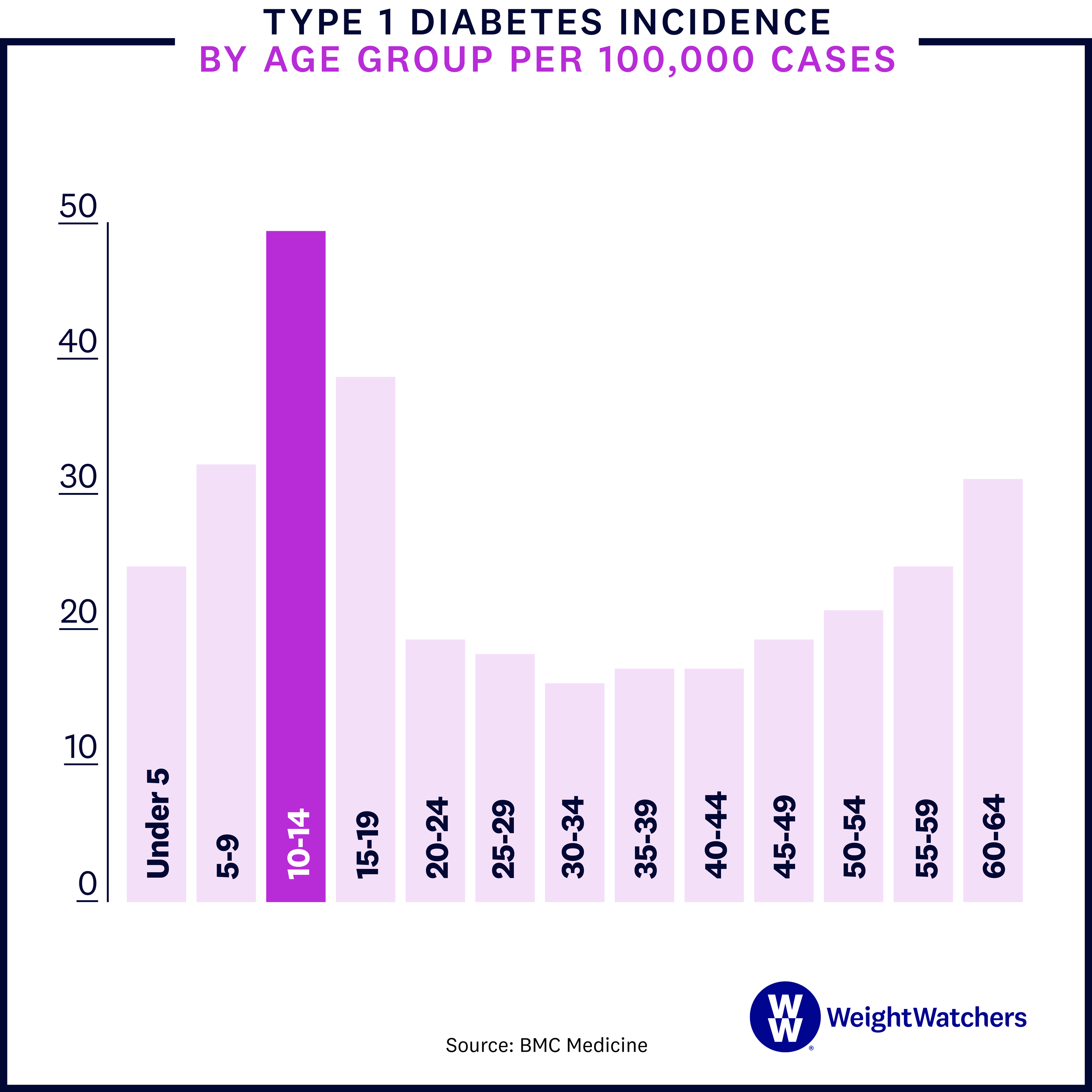
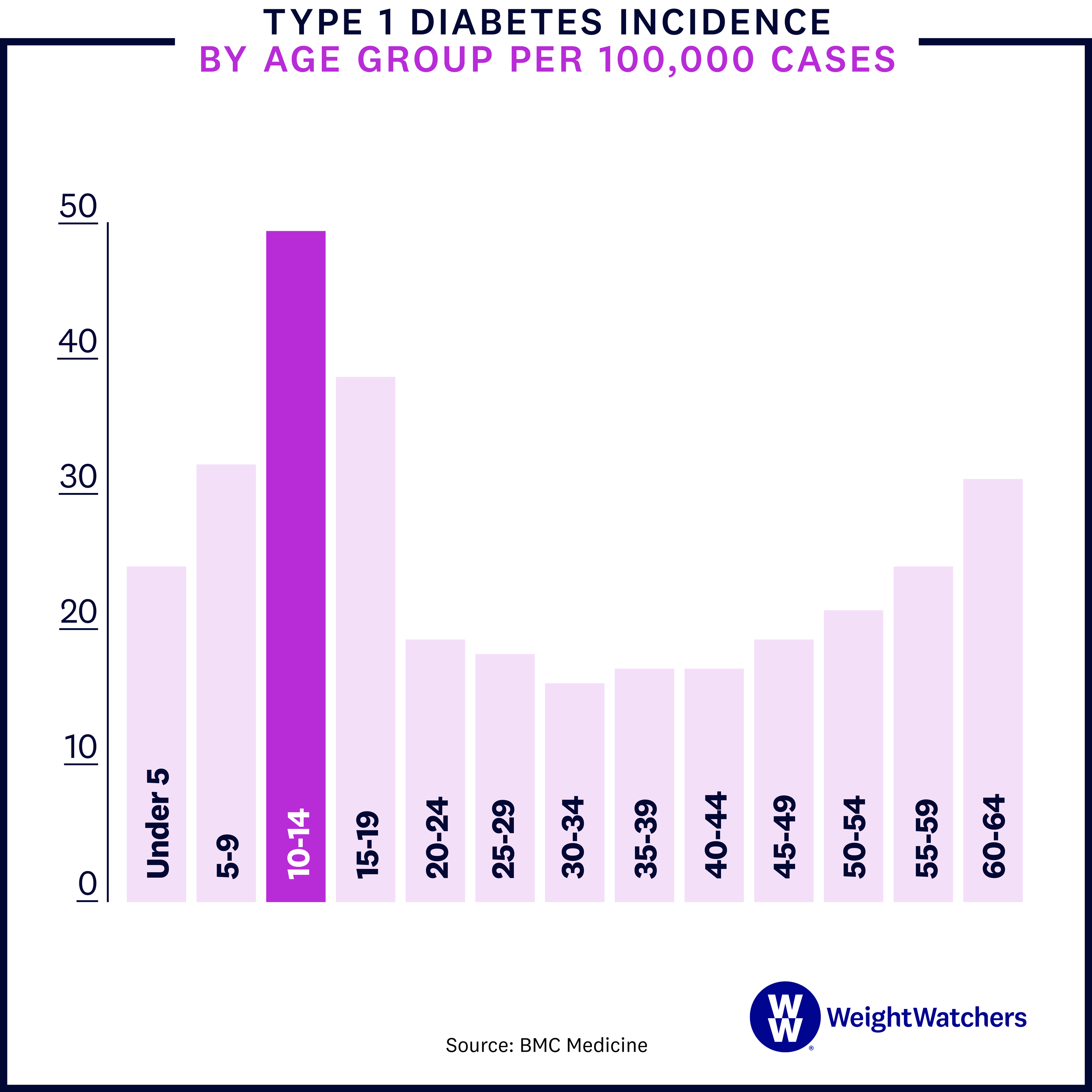
At what age are people usually diagnosed with type 1 diabetes?
Type 1 diabetes is sometimes called juvenile diabetes because it tends to be diagnosed in children and adolescents, but it can actually occur at any age. That said, the peak age for diagnosis is still between 10 and 14. And the number of diagnoses is growing: Among those under 20, the rates of T1D went up an alarming 45% from 2001 to 2017 (from 1.48 to 2.15 cases per 1,000 kids). Researchers are trying to figure out what’s behind that rise, part of a larger rise in autoimmune conditions.
What are the complications of type 1 diabetes?
Though T1D can be treated with insulin therapy (more on that below), the effect isn’t perfect. “It’s not possible to deliver insulin as precisely as the body would if all systems were working correctly,” Reusch says. As a result, blood sugar can stay elevated and lead to other conditions. In fact, close to 50% of people with type 1 diabetes will develop a serious complication within their lifetimes. Here’s a closer look at T1D complications.
- Ketoacidosis: Because people with poorly treated T1D have no way to turn glucose into energy, the body starts using fat as a source instead. The process of breaking down fat produces a waste product known as ketones, which can be toxic if levels get too high—a condition known as ketoacidosis. In severe cases, ketoacidosis can lead to coma and death. Check in with your doctor if you’re experiencing the below:
- Rapid breathing
- Fruity-smelling breath
- Nausea
- Vomiting
- Flushed face
- Stomach pain
- Dryness of the mouth
- Cardiovascular problems: Over time, high blood sugar can damage the blood vessels and nerves that control your heart. As a result, diabetes increases your risks of several cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis), and high blood pressure.
- Nerve damage (neuropathy): Excess blood sugar can injure the walls of the blood vessels (capillaries) that keep your nerves healthy. This can cause tingling, numbness, burning, or pain that tends to start at the tips of the toes or fingers and slowly spreads. In serious cases, this nerve damage can result in a foot needing to be amputated. If the nerve damage happens in the gastrointestinal tract, it can cause nausea, vomiting, diarrhea, or constipation.
- Kidney damage (nephropathy): High blood sugars can damage the blood vessels that filter waste in the kidneys. If the damage becomes severe, it may cause kidney failure or irreversible kidney disease, requiring dialysis or a kidney transplant.
- Eye damage: In time, too much blood sugar can block the tiny blood vessels that nourish the retina, cutting off its blood supply. Known as diabetic retinopathy, this condition can ultimately cause blindness. Diabetes can also up the risks of cataracts and glaucoma.
- Teeth and mouth conditions: Diabetes can impact saliva flow, which can cause dry mouth and, in time, gum disease.
- Pregnancy complications: High blood sugar levels while pregnant can increase the risks of miscarriage, stillbirth, preeclampsia (a serious condition that can occur halfway through pregnancy and is marked by high blood pressure and high protein levels in the mom’s urine), and birth defects.
How is type 1 diabetes treated?
The main form of treatment for T1D is insulin therapy, which is done in conjunction with regular blood glucose monitoring to watch blood sugar levels. “The inability of the pancreas to make enough insulin means that patients need insulin therapy to remain healthy,” says Dr. Tom Donner, M.D., an associate professor of medicine and the director of the Johns Hopkins Diabetes Center, in Baltimore.
Insulin is delivered via injection (either a needle or a pen) or an insulin pump, which is a wearable device. There are also different types of insulin, which vary by how quickly the medication acts. The type of insulin and dose you need depends on factors like your weight, activity level, diet, and whether you’re going through puberty, a pregnancy, or a sickness. Your doctor will advise you on the right type, amount, and schedule for your insulin therapy and monitor you regularly to make sure it’s working correctly.
The Risk of Type 1 Diabetes Complications Is Much Less If You…
Manage your glucose levels diligently with the help of your doctor
Research shows that people who had a period of intensive blood glucose control early on in their T1D diagnosis had a 30% lower risk of nerve problems, 49% lower risk of advanced diabetic eye disease, and 33% lower risk of advanced kidney disease in the decades that followed.
Keep your blood pressure down
Having high blood pressure doesn’t just raise your risks of heart attack and stroke; it is also associated with higher risks of kidney and eye damage. Symptoms aren’t obvious, so get your blood pressure checked regularly, and if it’s high, talk to your doctor about steps to take, like reducing your intake of sodium.
Exercise regularly
Research shows that being physically active lowers LDL cholesterol and reduces risks of cardiovascular disease and death in people with type 1 diabetes. Talk to your doctor about what types of activity might be best for you and how to manage your glucose when exercising.
What lifestyle changes can help manage T1D?
While exercise and diet are usually thought of as something people with type 2 diabetes need to worry about, movement and healthy food are also important for people with type 1 diabetes since lifestyle factors can impact blood sugar.
Activity
Exercise has been shown to improve glucose control, reduce the risk of cardiovascular disease, and improve well-being in people with T1D. While movement of any kind can be beneficial, research shows cardio is especially good at increasing cardiorespiratory fitness and decreasing insulin resistance. A couple of things to keep in mind:
Check in with your doctor first. Physical activity can affect blood sugar levels, so talk to your doctor to see if your carb intake and insulin doses should be altered before or after you work out. You may be told to up your carb intake or reduce insulin (or do both) to keep blood sugar in check.
The more you can move, the better. To see the biggest benefits, you’ll want to fit in 150 minutes or more of moderate- to vigorous-intensity aerobic activity weekly. Youths with type 1 diabetes should aim for 60 minutes of activity per day, the same recommendation for the general population.
Diet
“The type of food you choose, the amount you eat, and even the combination of food can affect your blood sugar and how fast it goes up or down,” says Barbra Sassower, RDN, a registered dietitian nutritionist and the certified diabetes educator at WeightWatchers®.
That’s why the WW Diabetes-Tailored Plan steers you away from foods that spike blood sugar, like those with refined carbs or added sugars, and toward foods that help steady it, like those rich in fiber, protein, and healthy fats. No detox, no cleanse, no carb counting—just balance.
