How obesity medicine specialists are changing weight treatment


Having stomach issues? Gastroenterologist. Patchy eczema? Dermatologist. Toothache? A dentist, obvi. It seems like there’s a specialist for virtually every health condition and body part. But what doctor should you see for weight management? Up until recently, there wasn’t one.
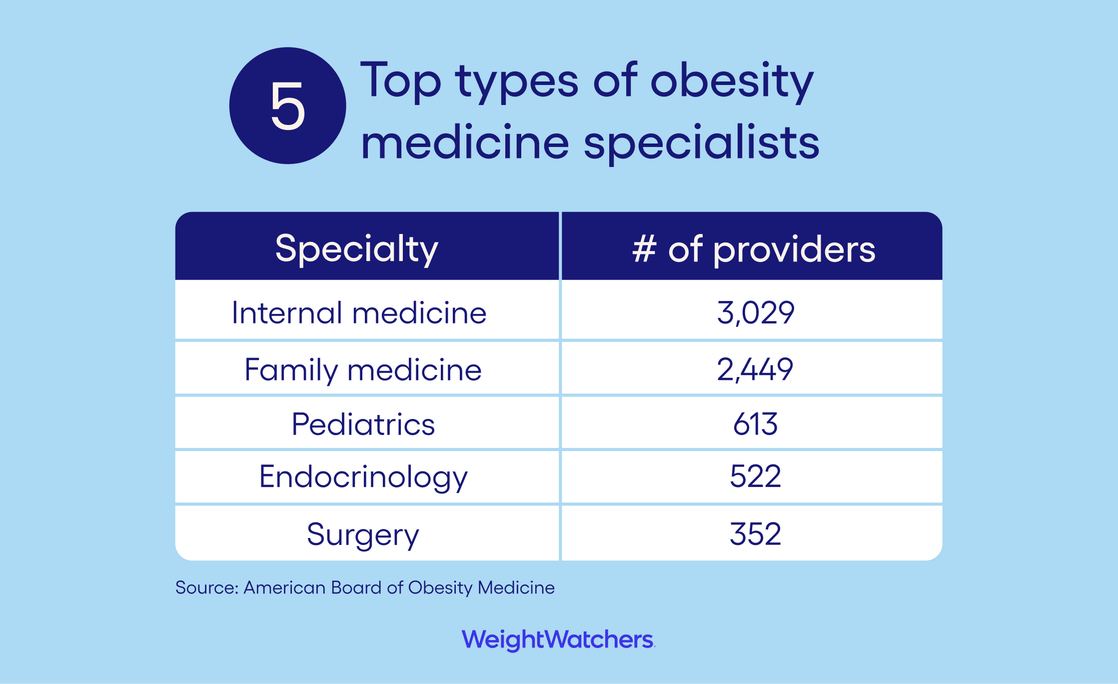
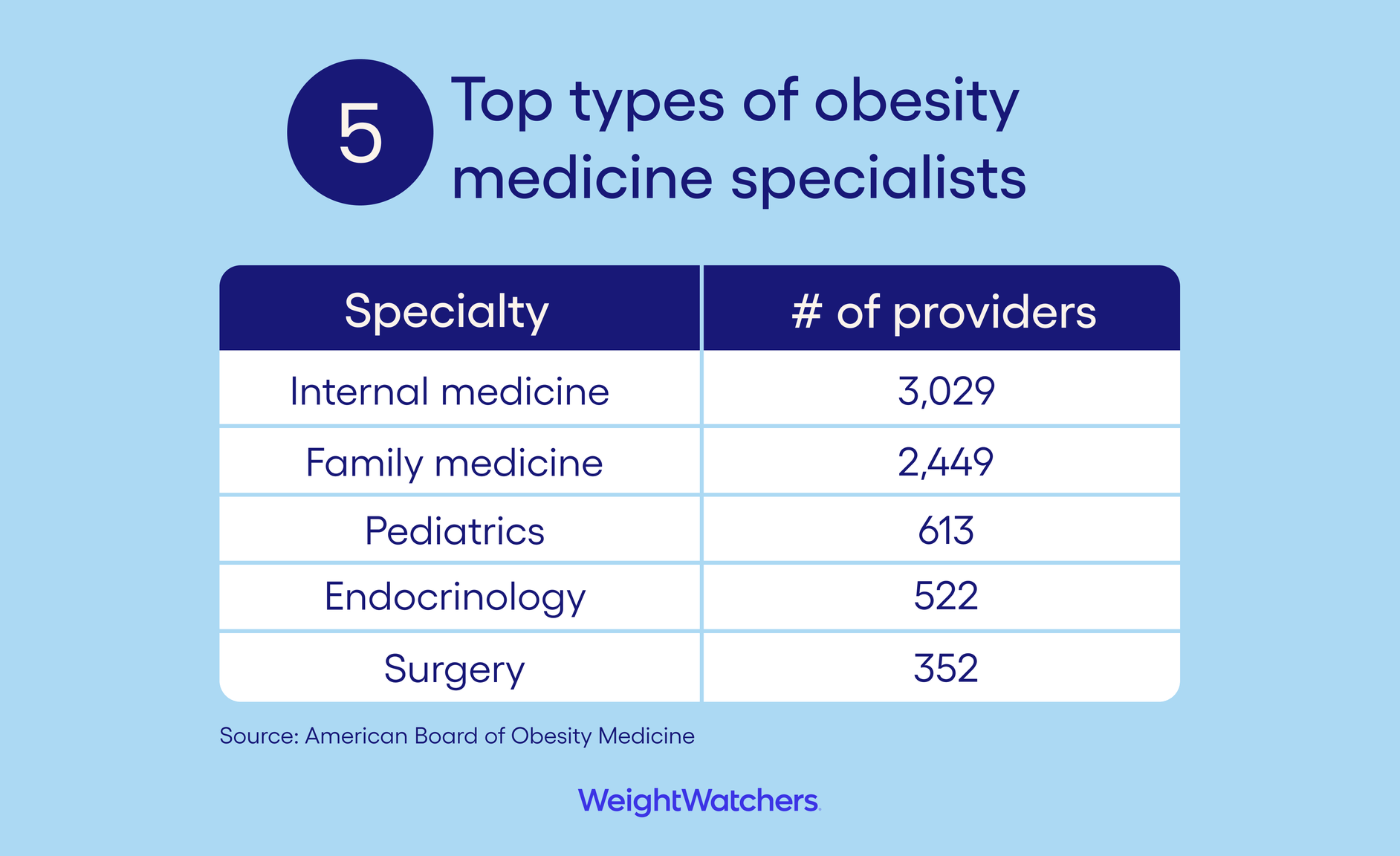
The American Board of Obesity Medicine, better known as ABOM, wasn’t established until 2011. Surprising, yes, but also understandable considering that obesity wasn’t formally recognized as a disease by the American Medical Association until 2013. And while the speciality may have started small, it didn't stay that way for long—the number of certified providers has almost doubled since 2020, and there are now more than 8,200. Here’s how seeing one of them could change your entire health journey, from diagnosis to treatment.
![quote: Understanding obesity is important to OBGYNs. It's important to surgeons. It's important to pediatricians. [This is a disease] that affects people in all healthcare settings. - DR. KIMBERLY GUDZUNE, M.D. MEDICAL DIRECTOR FOR THE AMERICAN BOARD OF OBESITY MEDICINE AND ASSOCIATE PROFESSOR OF MEDICINE AT JOHNS HOPKINS UNIVERSITY](https://v.cdn.ww.com/media/system/cms/us/Pullquote_Mobile_2.png?width=400&auto=webp&optimize=medium)
![quote: Understanding obesity is important to OBGYNs. It's important to surgeons. It's important to pediatricians. [This is a disease] that affects people in all healthcare settings. - DR. KIMBERLY GUDZUNE, M.D. MEDICAL DIRECTOR FOR THE AMERICAN BOARD OF OBESITY MEDICINE AND ASSOCIATE PROFESSOR OF MEDICINE AT JOHNS HOPKINS UNIVERSITY](https://v.cdn.ww.com/media/system/cms/us/Pullquote_Desktop_2.png?width=800&auto=webp&optimize=medium)
What is obesity?
While there is some controversy over how to define obesity, many health organizations rely on body mass index, or BMI. It’s a way to compare your weight to your height and is meant to determine when someone has excess body fat. If someone’s BMI is 30 or higher, they are classified in the obesity category. The classification doesn’t stop there, though. To help see the health risks associated with someone’s obesity, there are three different designations:
- Class 1 obesity: BMI 30 to <35
- Class 2 obesity: BMI 35 to <40
- Class 3, or severe obesity: BMI of 40 or higher
What is an obesity medicine specialist?
Obesity medicine specialists are providers who receive additional education and training in the treatment of obesity; often, they are certified by ABOM.
There are two ways to get those credentials. One pathway requires an additional year or more of clinical training in obesity medicine (i.e. a fellowship) after medical residency and passing a test administered by ABOM. But the most common pathway is for doctors to complete 60 hours of obesity-focused training and pass a test administered by ABOM, says Dr. Kimberly Gudzune, M.D., medical director for ABOM and an associate professor of medicine at Johns Hopkins University. “That pathway is really important, because we have a whole host of practicing physicians out in the community who never had the opportunity to learn about obesity in medical school, and we don’t want to tell them they need to stop their practice and go do a year-long fellowship.”
Other medical boards limit their certifications to specific types of doctors. (For example, only pediatricians can be certified by the American Board of Pediatrics.) Obesity medicine, on the other hand, is a specialty that all types of providers can pursue.
“Understanding obesity is important to OBGYNs. It’s important to surgeons. It’s important to pediatricians,” says Gudzune. “Obesity is a disease that affects people in all healthcare settings, and we’re trying to meet that need.”
Why the skillset is (increasingly) in demand
More than 40 percent of adults in the U.S. are living with obesity, and its prevalence increased by 10 percent in the last 20 years, according to the CDC. And yet: Most doctors get close to zero training in the disease. This may be because, unlike some other conditions, obesity impacts every single organ system in the body. “Medical schools would have to include obesity over and over again throughout the entire medical education experience, which simply doesn’t happen,” Gudzune says.
So more and more doctors are seeking to fill in the knowledge gaps that med school left behind. “I was only told in medical school to have patients work on eating better and working out to lose weight. That was the idea I left medical school with — that obesity is something people just need to work harder at to treat,” says Dr. Jennifer Ng, M.D., an internist and obesity medicine specialist at Mount Sinai Hospital in New York City. “I learned in my obesity medicine training that’s not the case. The right lifestyle doesn’t necessarily mean that you will lose weight.”
4 benefits of working with an obesity medicine specialist
Beyond the credentials, what sets an obesity medicine specialist apart from any other physician? Here are some specific areas where their in-depth training pays off for patients.
1. They understand the physiology of obesity. Up until recently, obesity was viewed as a behavioral issue. But obesity physicians see it on a cellular level too. “What determines your weight is very complex and involves the gut microbiome, hormones, and neurotransmitters in the brain, among many other things,” says Ng. “It’s a lot of different organ systems coming together.”
2. They’re up to speed on the latest science. “There are more and more treatment options, which is amazing,” says Gudzune. “But it’s also really overwhelming from a physician’s perspective.” Part of an obesity medicine physician’s job is to keep pace with a rapidly advancing field, so they can confidently “talk through a whole range of treatment options and the risks and benefits of each,” adds Gudzune.
3. They take the journey with you. You know those doctors you see once a year for a quick checkup? These are not those doctors. “Reaching your health goals is a marathon, not a sprint, and there will be hiccups and challenges along the way,” says Gudzune. “Having a partner there to support you and be your advocate is really key in having long-term success, which is why a lot of obesity medicine specialists try to see patients every four to six weeks.”
4. They just get it. Getting help for overweight or obesity takes a lot of courage — partly because people living with either condition know they risk facing discrimination. “Weight stigma and bias is incredibly common, and it also affects physicians,” says Gudzune. The problem is that some providers overcorrect to avoid it. “The increasing [awareness] of stigma and bias sometimes leads physicians to avoid bringing up obesity because they are worried it will make their patients feel stigmatized.” Obesity medicine specialists are trained in providing stigma-free, compassionate care without skirting the issue.
Who should see an obesity medicine specialist?
Because the word “obesity” is in the name of the specialty, you might assume these providers exclusively treat patients with a body mass index (BMI) over 30 — the measurement most health organizations use to distinguish the disease. But that isn’t actually true. They’re trained to care for any patient with health issues related to weight. “I work with patients whose BMIs would be in the overweight category, but they have every single complication related to the disease of obesity,” says Gudzune.
While it may seem scary to think that your obesity is serious enough to meet with a specialist about it, seeing one can make you feel much better about your health and your future. “In the majority of cases, patients are really happy to talk to me about their obesity,” says Ng. “They feel like they’ve been struggling for so long, that they have felt dismissed by the medical community or told they just aren’t working hard enough. They are happy to see someone who is willing to talk about their weight in a non-judgemental fashion.”
What to expect at your first visit
1. An intro to obesity: “I spend time talking about the term obesity and what it means,” says Gudzune. “It’s important to talk about how this is a medical diagnosis of a chronic condition.”
2. Your health history: This includes past and current medical conditions and medications. “If they have a history of an abnormal heart rhythm or kidney stones, for example, we wouldn’t choose certain weight-loss medications,” says Ng.
3. Your lifestyle: “I will ask them things like what physical activity they do, their sleep habits, and every single thing they ate over the last 24 hours,” says Ng. “Patients will try to please their doctors, so they may not want to tell me if they have eaten what they think is a ‘bad’ meal, but I really want to know.”
4. Your health goals: “We are going to treat you as a whole person, so we talk about getting you to your health goals, not just a number on the scale,” says Gudzune. In other words, you'll focus on achieving weight health, which is finding the right weight for you to optimize health and well-being.
5. Treatment options: “There is no one-size-fits-all approach to obesity, where everyone gets the exact same treatment plan,” says Gudzune. “We’ll have a back-and-forth discussion where we figure out together what you need.” This might include medical weight-loss offerings, like GLP-1 medications or bariatric procedures. Deciding the right path will be based on the specifics of your disease as well as personal preference. If your healthcare provider does decide to use a weight-management medication, they’ll know that it’s important to pair it with a healthy lifestyle for the greatest health benefits and results.
How to find an obesity medicine specialist
The rise in telehealth has made appointments with obesity specialists more accessible than ever. Take WeightWatchers’ telehealth clinic, for example. After taking a simple quiz to confirm eligibility for their medical weight-loss program, patients are paired with a board-certified clinician — all specially trained in obesity medicine, and the vast majority certified by ABOM.
For other options, you can search for nearby obesity specialists via ABOM’s “Find a Physician” tool. But you probably won’t be getting in to see one immediately. “For a lot of us, our practices are very popular, so you might need to wait a few months to get an appointment,” says Gudzune. This isn't true with providers at WeightWatchers Clinic, who often see patients within a couple of days.
The bottom line
For the past 10 years, physicians have been able to pursue extra training and become a certified obesity medicine specialist. This type of education can help fill in many of the gaps left after standard medical school, such as what really causes obesity, the latest treatment options, and the best way to reduce stigma and bias when talking to a patient with obesity. If you are living with overweight or obesity, consider making an appointment with an obesity medicine specialist to talk about your health today.
This content is for informational purposes only and does not constitute medical advice, diagnosis or treatment. It should not be regarded as a substitute for guidance from your healthcare provider.
WeightWatchers relies on only the most trustworthy sources, including highly credentialed experts, government and academic institutions, peer-reviewed studies, and respected medical associations. We focus on primary sources and research that is recent, relevant, and high-quality. For more about how we report, write, and fact check our stories, please see our editorial policy.
Obesity as a disease: Endocrinol Metab Clin North Am (2016). “Regarding Obesity as a Disease: Evolving Policies and Their Implications.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4988332/
Number of obesity medicine specialists: American Board of Obesity Medicine (2023). “Statistics and Data.” https://www.abom.org/stats-data-2/
Obesity statistics: Centers for Disease Control and Prevention (2022). “Adult Obesity Facts.” https://www.cdc.gov/obesity/data/adult.html
