What your BMI can (and can’t) tell you
It has been widely acknowledged for some time now that the body mass index (BMI) is an inaccurate tool for assessing someone's overall health and weight. Despite this, it is still being used as a measuring tool. What alternative methods could we use instead? We talked to experts about what you can and can’t learn from your BMI—and how to think about the number.
What is BMI?
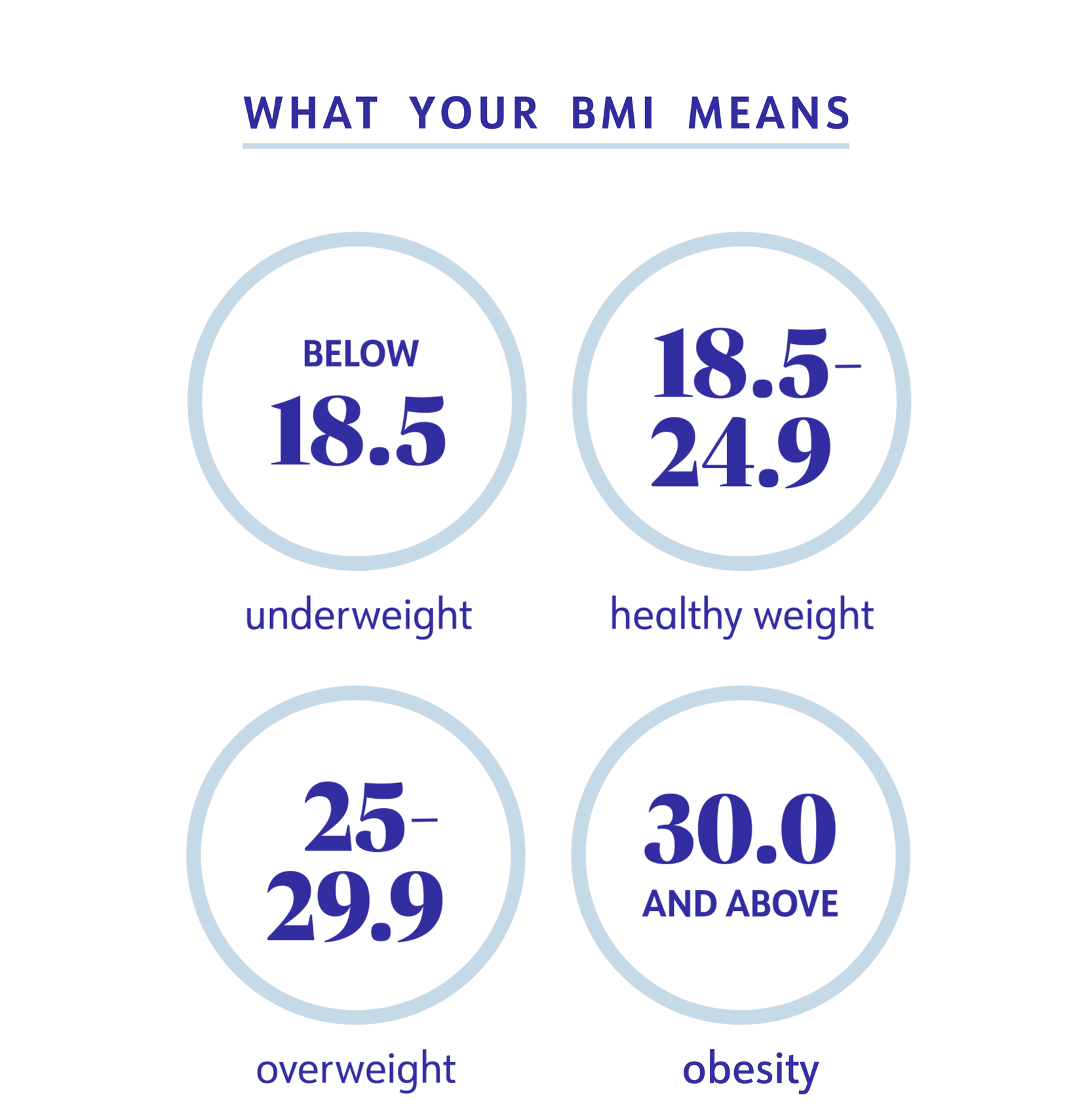
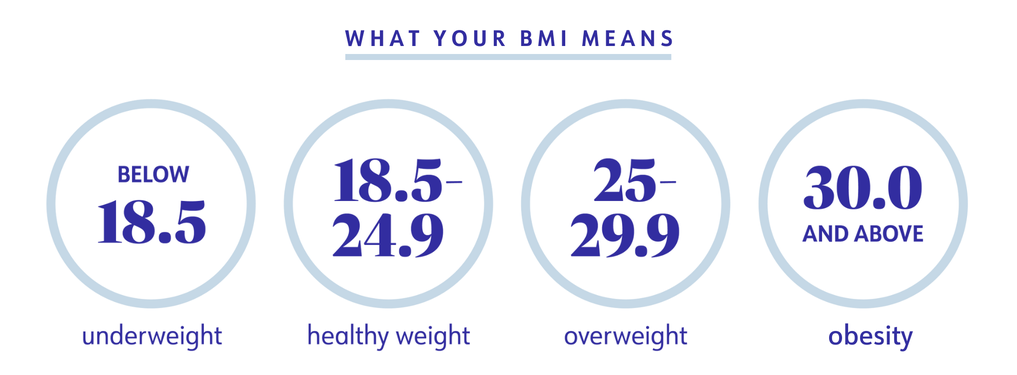
BMI, which stands for body mass index, is calculated by taking your weight in kilograms divided by the square of your height in metres—use an online BMI calculator to make it easy. The number you get correlates to different weight categories:
- Below 18.5: Underweight
- 18.5 – 24.9: Healthy Weight
- 25.0 – 29.9: Overweight
- 30.0 and above: Obesity
Obesity is further broken out into three categories:
- BMI 30 to 34.9: Class 1 obesity
- BMI 35 to 39.9: Class 2 obesity
- BMI 40 and higher: Class 3 obesity or severe obesity
What can BMI tell you about your health?
BMI was not invented for how it’s used today. It was created by a Belgian mathematician in the 1800s after he observed that weight tended to increase with one’s height. Then, in 1972, BMI was popularised by Ancel Keys, a physiologist who researched the link between saturated fat and heart disease. Keys found BMI to be the best way to measure obesity in his studies, and its use grew from there.
Let's make one thing clear: Obesity medicine experts say that BMI can give providers clues about what's going on in your body. That’s because having a higher BMI is correlated to having more body fat, and higher percentages of body fat can up your risk for certain diseases and conditions such as type 2 diabetes, osteoarthritis, many cancers, sleep apnea, and depression and anxiety, among others.
“When we talk about obesity, the issue at hand that’s contributing to the disease is adipose, or fat tissue,” says Dr. Amanda Velazquez, M.D., director of obesity medicine in the department of surgery at Cedars Sinai in Los Angeles, United States. “As someone gains more fat, there’s a low-grade cascade of inflammation.” That inflammation affects hormones, blood vessels, and your ability to regulate your weight. “Accumulating fat tissue causes more damage to your system,” says Velazquez.
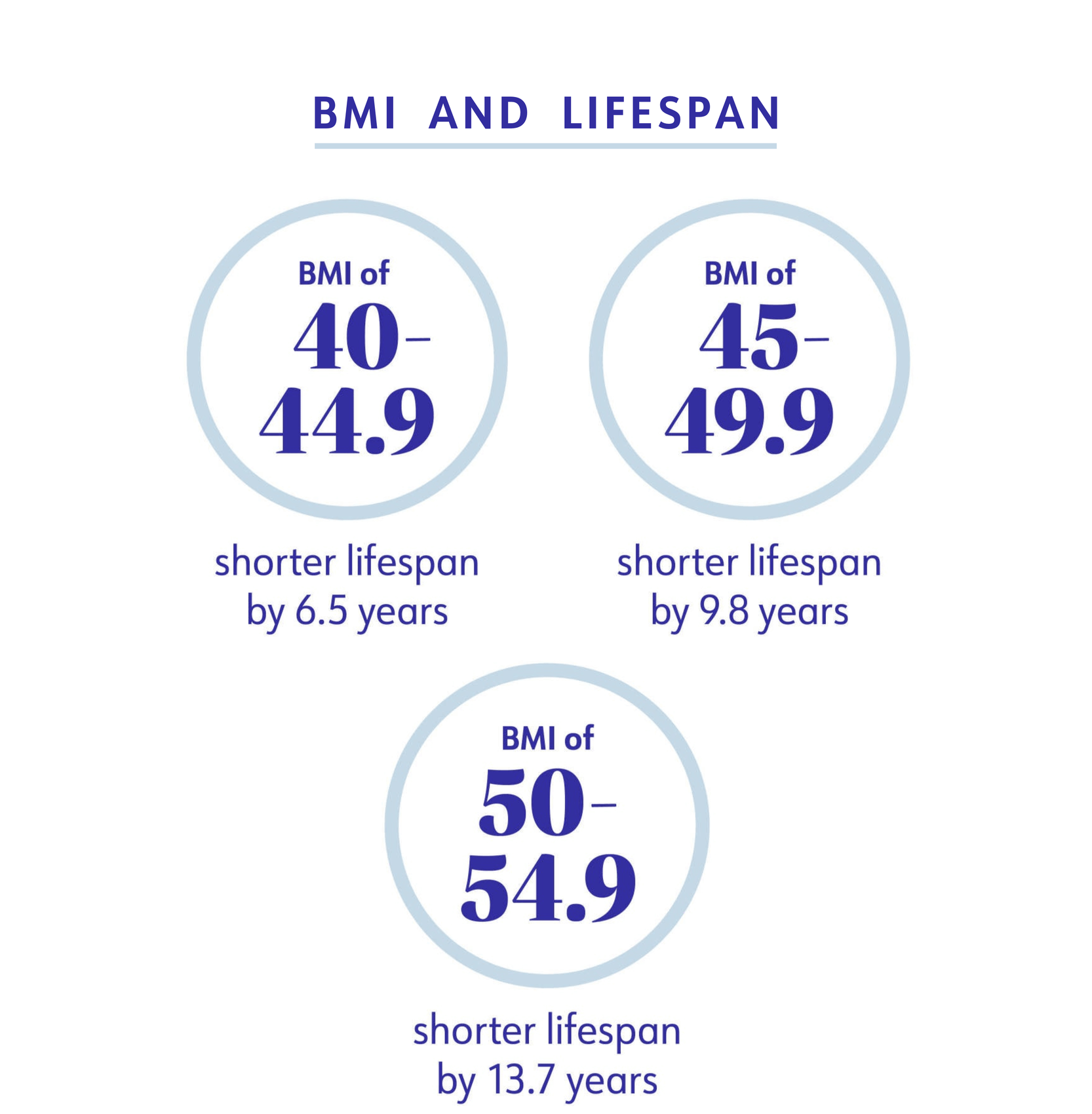
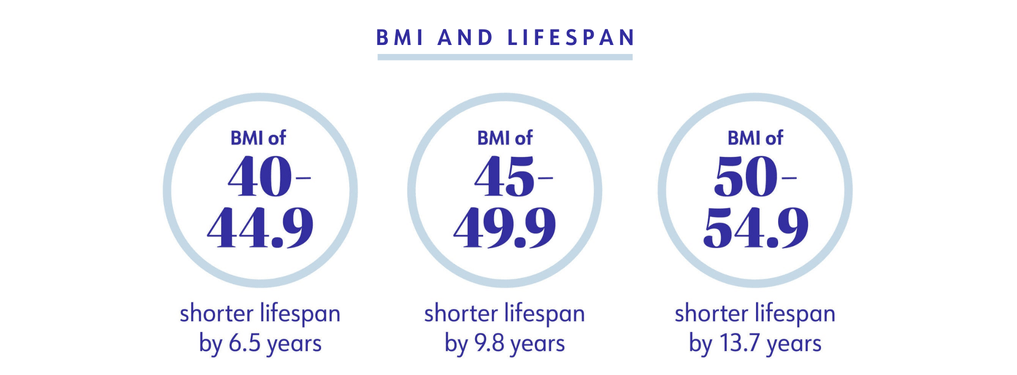
BMI is not something that can determine whether or not you have a certain disease, but it’s a breadcrumb providers use on the path to diagnosis. “BMI should be treated as a vital sign, like your blood pressure or pulse,” says Dr. Ethan Lazarus, M.D., past president of the American Obesity Medicine Association. It can help shine a light on some serious truths about your health. For example, Lazarus points to research that found that compared to people in the “healthy weight” BMI range, those with a BMI over 40 have much shorter lifespans:
- BMI of 40 to 44.9: a shorter lifespan by 6.5 years
- BMI of 45 to 49.9: a shorter lifespan by 9.8 years
- BMI of 50-54.9: a shorter lifespan by 13.7 years
“At the really high BMI ranges, the number correlates to health risk,” he says.
It’s also worth noting that while just 1.6% of adults are underweight, BMI can help flag when someone’s weight is too low and they’re at risk for certain conditions. For example, having a low body mass index can contribute to menstrual irregularities, problems getting pregnant, osteoporosis, anaemia, and depression, according to the American Office on Women’s Health.
What can’t BMI tell you about your health?
One of the big criticisms of BMI is that it’s not that useful on an individual level. While it’s helpful when performing large research studies to compare health risks across populations (it lets you remove height as a factor when comparing things, such as the link between weight and type 2 diabetes risk in a group of 10,000 people), any one person’s BMI doesn’t tell much about their health. In other words, it can’t help providers see if they have high blood pressure or are developing heart disease.
Another issue is that modern-day cut-off points for healthy weight, overweight, and obesity have been criticised as being random. Is a BMI of 29.8 a lot less healthy than a BMI of 30.2? No, but like many other health statistics (cholesterol levels, blood pressure, and more), cutoffs have to happen somewhere. “We know as BMI increases, there is a higher risk for certain diseases,” says Velazquez.
The fact that BMI ranges are the same for almost everyone—regardless of factors like age, activity level, sex, and race or ethnicity—is a major limitation. This can make it easy to overlook nuances related to the weight-health connection in different groups of people. The Asia-Pacific classification of BMI has a lower cutoff for overweight and obesity categories (overweight starts at 23 and obesity at 27), because research shows they have increased health risks at lower BMIs than people of other races or ethnicities.
“You have to interpret BMI in the context of the individual,” says Lazarus. Are you a professional athlete who has a lot of muscle mass? Then you may have a falsely high BMI even though you aren’t at a higher risk for weight-related chronic diseases. Those factors can be missed when you’re using a single number to determine health, so it’s important to have the full picture and not just rely on BMI as the sole marker for health.
"You have to interpret BMI in the context of the individual."— Dr. Ethan Lazarus, M.D.
Why do providers still use BMI?
“BMI can be used alongside other measures, such as waist circumference, quality of life surveys, functionality, and the presence of other medical conditions related to weight, like high blood pressure and diabetes,” says Velazquez. And if your BMI is moving up alongside markers for chronic health conditions or affecting your quality of life, you and your healthcare provider can have a conversation about it and figure out the right path forward.
Other measurements, such as skinfold thickness, underwater weighing, or DXA scans, can be used as more direct measurements of body fat, but each has pros and cons. While skinfold thickness measurements may be accessible in places like fitness centres, DXA or underwater weighing are more accurate and more often used in a clinical setting but can be more difficult to access.
WeightWatchers® also still uses BMI, but only to ensure members aren’t aiming for a weight that’s too low for their height. It’s not used in any other way to help members set goal weights.
So, how much importance should you place on BMI?
While BMI is still a controversial measure, Velazquez says she strongly encourages people to have their BMI calculated by their healthcare provider. “[It’s] not the most precise or accurate tool when it comes to being a marker of our health, but it’s a tool in our toolbox,” she says. “It just shouldn’t be used as the only indicator of someone’s health.”
What your BMI means for your health tends to correlate to what weight category it falls in. Here’s how that looks:
If your BMI is in the overweight category (25.0 – 29.9)
The next step, says Lazarus, “is to look at the health impact of your BMI.” Your healthcare provider will check for high cholesterol or hypertension, for instance. Also, think about your body functionality—is there anything you can't do because of your weight, such as play on the floor with your kids or garden?
If a patient’s BMI is over 25, Lazarus also likes measuring a patient’s waist circumference, which is a marker of visceral fat (the type of fat that surrounds your organs and causes inflammation). Government guidelines say men should have a waist circumference of less than 94 cm, while women should have one less than 80 cm. If your BMI is in the overweight category and your waist is larger than these numbers, your healthcare provider may recommend a weight management treatment plan, including lifestyle changes, to decrease your body fat.
If your BMI is in the class 1 obesity category (30 to 34.9):
A BMI between 30 and 34.9 is linked to type 2 diabetes, fatty liver disease, and reduced life expectancy, as well as stigma and discrimination. “If you develop the chronic disease of obesity, we want to treat it,” says Lazarus. “Not many people have a BMI of 30 that’s not starting to impact their health.”
What’s more, “we know that for people who have an elevated weight and normal health markers, it’s only a matter of time before problems develop,” adds Velazquez. That’s why intervening early is important instead of just waiting–you can possibly prevent the complications of obesity.
It’s approximately near this 30-plus number that experts say you should also consider obesity treatment, which may include lifestyle changes and medical interventions, such as medication. Bariatric surgery may also be recommended for people who have a BMI over 35 or a BMI over 30 along with type 2 diabetes that is difficult to control.
If your BMI is in the class 2 or 3 obesity category (35+)
Once your BMI goes above 35, it’s associated with a six- or 10-fold higher risk, respectively, for developing what’s called “complex multimorbidity,” which is having four or more chronic diseases like diabetes, hypertension, and osteoarthritis.
Lazarus says that it’s difficult to bring BMI down to a normal level through lifestyle changes alone with higher levels of obesity. But, a healthy diet and exercise combined with an TGA-approved weight management medication can result in a 10 to 15 per cent weight loss, he says. Don’t focus on whether or not that amount of weight loss will get your BMI down into the “healthy weight” category. Remember: the goal is to improve your health, not get to a number on a chart.
Losing 5% to 10% of your body weight likely will improve your blood pressure, blood cholesterol, and blood sugars. “If you reduce your body weight by 5%, you’ve also reduced your BMI by 5%. We know at that point, you’re starting to improve your health and risk of comorbidities,” Lazarus says. However, he encourages patients with obesity to aim for a 10% to 20% weight loss, and “we have the tools to do it today.” The WeightWatchers Points Program is sustainable and will help you create healthy habits that lead to long term weight loss through science-backed behaviour change.
BMI’s possible successor
If there’s anything that can replace BMI in the future, it’s likely going to involve your waist circumference. Research shows that body fat distribution—especially belly fat—is more indicative of health than BMI. For example, one new study shows that waist-to-hip ratio is a more accurate way of determining who is at risk for obesity-related health complications than BMI.
It isn’t the go-to method right now—waist measurements can take a little extra time to perform during a healthcare provider’s visit and practitioners may not understand it as well as they do BMIs. But more and more experts, including Lazarus and Velazquez, are recommending it. If you do have your waist measured, it can be used alongside your BMI to assess your risk for obesity-related conditions.
The bottom line
Interpret your BMI through the lens of your overall health and think of it as only one of the many tools that can measure it. “Diminishing the value of BMI is hurting—not helping—us,” says Velazquez. “I think it has inherent flaws that we recognise, but as a medical professional, we want to be able to have all of the information in front of us to make the best shared medical decision with the patient.”
What is BMI: Centers for Disease Control and Prevention. (2022). “About Adult BMI.” https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
BMI Calculator: Centers for Disease Control and Prevention. (2022). “Adult BMI Calculator.” https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/english_bmi_calculator/bmi_calculator.html
BMI and percentage of fat: Centers for Disease Control and Prevention. (2022.) “About Adult BMI.” https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
Health and overweight and obesity: Centers for Disease Control and Prevention. (2022). “Health Effects of Overweight and Obesity.” https://www.cdc.gov/healthyweight/effects/index.html
Underweight statistics: Centers for Disease Control and Prevention. (2020). “Prevalence of Underweight Among Adults Aged 20 and Over: United States, 1960-1962 Through 2017-2018.” https://www.cdc.gov/nchs/data/hestat/underweight-adult-17-18/underweight-adult.htm
Underweight risks: Office on Women’s Health. (2021). “Underweight.” https://www.womenshealth.gov/healthy-weight/underweight
History of BMI: International Journal of Epidemiology. (2014). “Commentary: Origins and evolution of body mass index (BMI): continuing saga.” https://academic.oup.com/ije/article/43/3/665/2949550
Waist circumference: Centers for Disease Control and Prevention. (2022).” Assessing Your Weight.” https://www.cdc.gov/healthyweight/assessing/index.html
Lifespan and obesity: PLOS Medicine. (2014). “Association between class III obesity (BMI of 40-59 kg/m2) and mortality: a pooled analysis of 20 prospective studies.” https://pubmed.ncbi.nlm.nih.gov/25003901/
Bariatric surgery and health risks: Journal of Medicine. (2013). “Review of the key results form the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery.” https://onlinelibrary.wiley.com/doi/full/10.1111/joim.12012
Severe obesity health risks: The Lancet Diabetes & Endocrinology. (2022). “Body-mass index and risk of obesity-related complex multimorbidity: an observational multicohort study.” https://www.thelancet.com/journals/landia/article/PIIS2213-8587(22)00033-X/fulltext
Weight loss benefits: Centers for Disease Control and Prevention. (2022). “Losing Weight.” https://www.cdc.gov/healthyweight/losing_weight/index.html
Bariatric surgery: National Institutes of Diabetes and Digestive and Kidney Diseases. (2020). “Potential Candidates for Weight Loss Surgery.” https://www.niddk.nih.gov/health-information/weight-management/bariatric-surgery/potential-candidates
Body fat measures: Centers for Disease Control and Prevention. (2022). “Defining Adult Overweight & Obesity.” https://www.cdc.gov/obesity/basics/adult-defining.html
Waist-hip ratio: European Heart Journal. (2023). “Anthropometric measures and adverse outcomes in heart failure with reduced ejection fraction: revisiting the obesity parados.” https://academic.oup.com/eurheartj/article/44/13/1136/7072269
