The most important things to know about type 2 diabetes


What is type 2 diabetes?
Affecting almost 1.3 million Australians, type 2 diabetes results from something called insulin resistance. Insulin is a hormone released by the pancreas that’s essential for ferrying glucose (sugar) from the bloodstream to cells throughout the body, where it’s used for energy.
In type 2 diabetes, however, the body requires more and more insulin just to get glucose out of the blood. The pancreas can’t keep up with the rising demand. The result is high blood sugar, the overlapping feature of all diabetes types. Over time, that can lead to a variety of complications, including nerve damage and kidney disease.
What causes type 2 diabetes?
There isn’t a single diabetes cause or trigger that makes someone develop insulin resistance. But there are a number of factors that can raise someone’s risk:
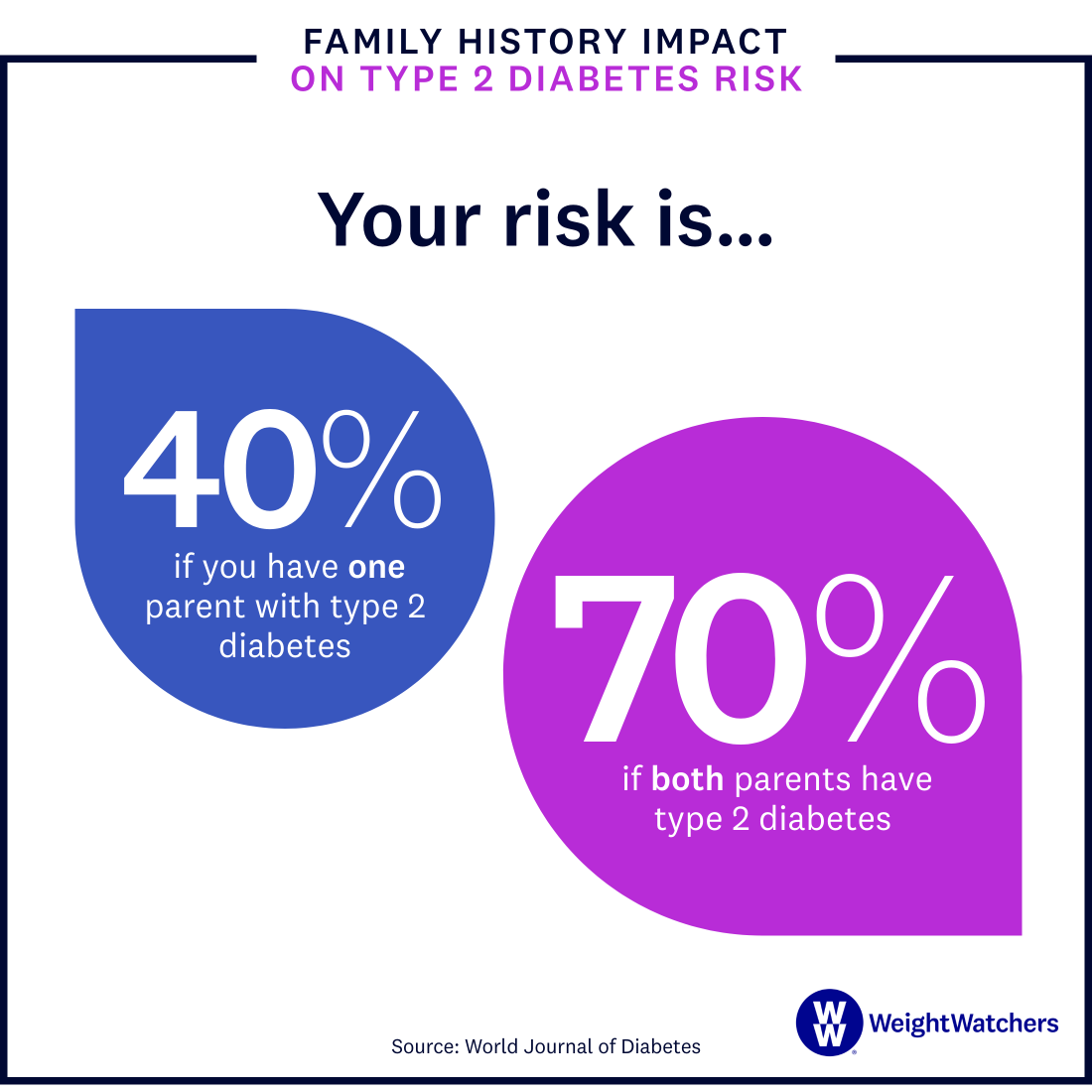
- Genetics. People can be born with a predisposition to insulin resistance and impaired insulin production, and therefore type 2 diabetes. The condition is more likely to occur in those who have a family history of it, says Jane Reusch M.D., a professor of medicine, bioengineering, and biochemistry and the associate director of the Ludeman Family Center for Women’s Health Research at the University of Colorado, United States.
- Weight. Obesity is linked to 30% to 53% of new type 2 diabetes cases every year. Having overweight or obesity can make it harder for glucose to get into cells—leading to insulin resistance. A type of body fat known as visceral fat, which surrounds internal organs and causes inflammation throughout your body, also raises the risk of insulin resistance.
- Inactivity. When you’re physically active, your body is more sensitive to insulin, meaning it moves glucose in the blood more efficiently. Also, having more muscle mass helps your cells take in more glucose for energy. Being inactive—defined as not doing anything physical during leisure time for the past month—means you’re missing out on those benefits, which raises your risk of insulin resistance.
- Age. The majority of people who are diagnosed with type 2 diabetes are over the age of 45. This is likely because you tend to lose muscle mass and gain fat as you age, says Reusch. “These are two of the critical components that impact insulin resistance and risk for developing type 2 diabetes.”
- Sex. Men are more likely to get type 2 diabetes than women. This is likely because as men get older, they carry more fat in their bellies—typically visceral fat—which is a risk factor.
- Socioeconomic status. Diabetes has been shown to disproportionately affect those in low-income populations, a trend tied to disparities in things like access to healthcare, healthy food, and spaces to exercise safely.
- Race. The disparities that apply to socioeconomic status also apply to marginalised racial and ethnic communities. The risk of type 2 diabetes is higher for these individuals due to factors like decreased access to healthcare and higher levels of stress.
What are the symptoms of type 2 diabetes?
Signs of type 2 diabetes often develop slowly. In fact, you can be living with type 2 diabetes for years and not even know it (a big reason why it’s undiagnosed in 23% of people with the disease). When signs and symptoms are present, they may include:
- Increased thirst
- Needing to urinate more frequently
- Increased hunger
- Unexplained weight loss
- Fatigue
- Blurry vision
- Sores that heal slowly
- Frequent infections
- Feeling numbness or tingling in the hands or feet
- Developing areas of darkened skin, usually in the armpits and neck
How is type 2 diabetes diagnosed?
To be officially diagnosed with type 2 diabetes, your doctor will perform one of several tests that measure blood sugar levels.
Glycated Haemoglobin (A1C) Test: This blood test indicates your average blood sugar level for the last two to three months. A reading of 6.5% or higher indicates diabetes.
Random Blood Sugar Test: For this test, blood sugar is measured in millimoles of sugar per litre of blood (mmol/L). A level of 11.1 mmol/L or higher suggests diabetes, especially if you also have symptoms, such as frequent urination and extreme thirst.
Fasting Blood Sugar Test: If your blood sugar is 7 mol/L or higher after an overnight fast on two separate tests, you’ll be diagnosed as having type 2 diabetes.
What are the complications from type 2 diabetes?
Over time, high blood sugar can affect many of your major organs, including your heart and kidneys, as well as nerves and blood vessels. This puts people with type 2 diabetes at risk of issues like heart disease, eye damage, and more.
- Cardiovascular disease hits people with diabetes hard: They are twice as likely to have heart disease or stroke than someone without diabetes. Over time, high blood sugar can damage blood vessels and the nerves that control your heart. People with diabetes are also prone to high blood pressure, high LDL cholesterol, and high triglycerides—all of which increase the risk of heart disease.
- Eye damage (retinopathy) is common since high blood sugar can damage the blood vessels of the retina, cutting off the blood supply. Type 2 diabetes can also lead to other serious eye diseases, such as cataracts and glaucoma.
- Nerve damage in limbs (neuropathy) happens when prolonged high blood sugar damages or completely destroys nerves, resulting in tingling, numbness, burning, pain, or total loss of feeling in the toes and fingers.
- Kidney damage (nephropathy) occurs when excess glucose damages the blood vessels that filter waste in the kidneys. Diabetes can lead to chronic kidney disease or irreversible end-stage kidney disease, which often requires dialysis or a kidney transplant.
How can you prevent type 2 diabetes?
Between 78% and 83% of new type 2 diabetes cases could be avoided by adopting a healthier lifestyle, including the following:
- Losing weight. If you have overweight, losing just 5% of your body weight can help prevent type 2 diabetes. For someone who weighs 90 kilograms, that would mean a 4.5 kilogram weight loss.
- Moving more. Physical activity helps control blood sugar and weight while improving blood pressure and cholesterol—all risk factors for developing type 2 diabetes. And you don’t need to hit the gym hard either. According to the American National Institutes of Health, just 30 minutes of walking, or other low-intensity exercise daily, combined with a low-fat diet, reduces the risk of developing type 2 diabetes by 58%.
- Eating healthily. To reduce your risk of type 2 diabetes, pack your plate with non-starchy vegetables, fruit, lean protein, and wholegrains as much as possible. Try to limit processed foods, trans fat, and sugary drinks.
How is type 2 diabetes treated?
Your doctor will work with you to create a tailored diabetes treatment plan, which may include oral medication to help the body use insulin more effectively or increase insulin production. If your blood sugar is still difficult to control with oral medications, your doctor may also suggest insulin therapy, which involves injecting insulin at specific points during the day.
Tell me more about... diabetes medications
Q: Does everyone with type 2 diabetes need to take medication?
A: “No they don’t—you can control type 2 diabetes with weight loss,” says David Marrero, Ph.D., director for the Center for Border Health Disparities at the University of Arizona in Tucson and former President, Health Care and Education of the American Diabetes Association. “But I don’t want to give false hope: You have to be willing to make pretty significant lifestyle changes with diet and exercise to lose enough weight that you can completely avoid medication.”
Q: What should you say to your doctor if you want to try losing weight first?
A: “Sustained high glucose can cause a bunch of problems, so many doctors will pull the trigger and start you on medication right away,” says Marrero. “But it’s not unreasonable to tell your doctor that you want to try to lose a certain amount of weight and come back and be tested again before starting medication. If you do lose weight and still aren’t controlling glucose adequately, your doctor can always start you on medication then.”
Q: If you start medication, can you go off it by losing weight down the road?
A: “Yes, you can, but it depends on what your body is doing and how well it’s dealing with glucose,” says Marrero. “Even if you don’t stop all medication, you can still improve your diabetes. There are people who start at one dose and reduce it significantly because they’ve lost weight.”
What lifestyle changes can help type 2 diabetes?
Medications can be helpful, but lifestyle modifications are key. “Nutrition and physical activity are central to the management of type 2 diabetes,” Reusch says. Losing weight and keeping it off through healthy habits can even help type 2 diabetes go into remission, which is when glucose levels return to nondiabetic ranges and stay there for at least six months, with no diabetes medications.
The food you eat is especially important since it has a direct impact on how often your blood sugar spikes. For example, eating fewer refined carbohydrates, including added sugars, makes it easier to manage glucose.
There’s no one-size-fits all diet plan for those with diabetes. That’s why the WeightWatchers® diabetes program offers a personalised weight-loss regimen that takes your condition into account along with your goals and your favourite foods—and it’s proven to work, lowering both body weight and blood sugar levels.
This content is for informational purposes only and does not constitute medical advice, diagnosis or treatment. It should not be regarded as a substitute for guidance from your healthcare provider.
https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
https://diabetes.org/tools-support/diabetes-prevention/high-blood-sugar
https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/diagnosis-treatment/drc-20351199
https://www.cdc.gov/diabetes/data/statistics-report/index.html
https://onlinelibrary.wiley.com/doi/full/10.1111/dme.14639
https://newsroom.heart.org/news/obesity-contributes-to-up-to-half-of-new-diabetes-cases-annually-in-the-united-states
https://my.clevelandclinic.org/health/diseases/22206-insulin-resistance
https://www.niddk.nih.gov/health-information/diabetes/overview/risk-factors-type-2-diabetes
https://diabetes.org/diabetes/cardiovascular-disease
https://www.cdc.gov/diabetes/library/features/diabetes-and-heart.html
https://www.cdc.gov/diabetes/managing/problems.html#
https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/achieving-type-2-diabetes-remission-through-weight-loss
https://cdc.gov/diabetes/library/features/diabetes-and-heart.html
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0176615
https://niddk.nih.gov/health-information/diabetes/overview/preventing-type-2-diabetes
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3109209/
https://diabetesjournals.org/care/article/39/11/2065/37249/Physical-Activity-Exercise-and-Diabetes-A-Position
https://niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes
https://diabetes.org/healthy-living/recipes-nutrition/understanding-carbs
https://pubmed.ncbi.nlm.nih.gov/27490920/#
https://archive.cdc.gov/www_cdc_gov/media/releases/2020/0116-americas-inactivity.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6389265/
