Diabetes symptoms and signs


What is diabetes?
Affecting around 1.8 million Australians and ¼ million New Zealanders, diabetes mellitus (the formal name) is a chronic disease caused by too much glucose, or blood sugar, circulating in your body. This can be caused by one of two things: Either your pancreas doesn't produce enough insulin (a hormone that regulates blood sugar), or your body can’t properly use the insulin it has (something known as insulin resistance). Insulin's job is to carry glucose to your cells for energy. When it doesn’t, you end up with too much glucose in your blood, triggering inflammation and ultimately organ damage.
A quick refresher on four distinct types:
- Type 1 diabetes: This is an autoimmune condition that causes the pancreas to stop producing enough insulin.
- Type 2 diabetes: By far the most common type, this is when your pancreas may produce enough insulin, but your body can’t use it properly.
- Gestational diabetes: As with type 2, your body can’t use its insulin supply—but this occurs only temporarily during pregnancy.
- Prediabetes: This is a condition where blood sugar levels are elevated, but not high enough to qualify as diabetes.
What are the signs of diabetes?
Diabetes symptoms tend to fly under the radar—so, it's possible you won't experience any signs. In fact, it's estimated that one in five people with diabetes have no idea that they have it. “For many, by the time you start getting symptoms, your diabetes may have been around for months or even years,” says Dr. Shabina Ahmed, M.D., an endocrinologist and an Assistant Professor of Medicine at Johns Hopkins University, in Baltimore, United States.
That said, there are some common signs to keep an eye on for type 1 and type 2 diabetes. If you notice any of the following, discuss it with your doctor.
- Frequent urination: With diabetes, your kidneys go into overdrive trying to get rid of the excess glucose, so you end up making a lot more trips to the bathroom. "When your blood sugar levels are consistently elevated above around 180 to 200 mg/dL (milligrams per deciliter), your body starts transferring glucose into the urine,” says Dr. Joshua D. Miller, M.D., the Medical Director of Diabetes Care at Stony Brook Medicine and an Associate Professor of endocrinology and metabolism at Stony Brook University, in New York. “The glucose brings water with it, and you have to pee out all that water.” The condition that produces this glucose-water mix is called polyuria, and it's often an early sign in children with type 1 diabetes, especially if they used to stay dry at night and are suddenly soaking their nappy or wetting the bed, says Miller.
- Excessive thirst: This isn’t a simple craving for water. Known as polydipsia, it's more of an unquenchable thirst—think big gulp–size. “As you become more dehydrated from the frequent urination, your sodium levels go up and the thirst mechanism kicks in,” says Miller. The hypothalamus (the part of your brain that regulates thirst) tells your body to crave as much fluid as possible so that it can replace the water your kidneys are using to flush out the glucose. The result: You drink and drink but never feel hydrated.
- Increased hunger: When your body can't convert glucose into energy, you get hungry. Really hungry. This is known as polyphagia.
- Extreme fatigue: Not enough energy in your cells can leave you feeling pretty sluggish and lethargic. (And dehydration can make that even worse.) A study found that 68% of people with type 2 diabetes experienced fatigue. (And it can happen with type 1 as well.)
- Tingling, pain, or numbness in the hands or feet: Also known as diabetic neuropathy, these symptoms occur when high blood sugar damages the nerves that send signals to the hands and feet. Most people notice this in the feet first and then in the hands as the disease progresses, says Ahmed.
- Wounds that won't heal: Over time, diabetic neuropathy, which is most common in hands and feet (see above), leads to a reduced sensation of pain. So you could stub your toe (hard!) and not feel a thing. For people with diabetes, this only opens the door for additional complications. Research shows that the inflammation brought on by uncontrolled diabetes impacts your body’s natural healing process by slowing down blood circulation and the delivery of wound-healing nutrients. In short, sores and cuts take an extra-long time to heal. “This is a symptom I tend to see most,” says Barbra Sassower, RDN, a registered dietitian and WeightWatchers® certified diabetes educator. “Patients don't know they have diabetes, but they have this foot wound that won't go away.”
- Unexplained weight loss: When your body doesn't get the energy it needs from glucose, it turns to fat and muscle instead, resulting in weight loss. It's more common with type 1 diabetes but can occur with type 2 as well.
What are the more unusual symptoms of diabetes?
While they aren’t as common as the symptoms listed above, doctors do sometimes see the following unusual symptoms in people with diabetes.
- Irritability: Anger, anxiety, and even depression have been associated with poorly regulated blood sugar—which is the crux of diabetes. The exact reason why remains unclear. A recent review published in Endocrinology, Diabetes & Metabolism determined that more research is needed to better understand the link between glucose and mood.
- Recurrent infections: Elevated blood sugar levels that are left unchecked can weaken your immune system, leading to a higher risk of infections. Research shows that the urinary tract becomes especially infection-prone in those with type 2 diabetes since the higher levels of glucose in the urine can promote bacterial growth.
- Itching: High blood sugar dries out your skin (a side effect of dehydration caused by excessive urination), which can leave it dull, flaky, and itchy.
- Acanthosis nigricans: A dark patch appearing on the skin with a velvety texture (especially the neck, armpits, or groin) is an indicator of insulin resistance. “This sign usually comes before a type 2 diabetes diagnosis,” Ahmed says.
- Skin tags: Small growths on the neck, eyelids, armpits, or groin can indicate type 2 diabetes. This is due to insulin levels that are higher than they should be. “Insulin can act as a growth factor, and skin tags form from an overgrowth of skin cells,” Ahmed says.
- Fruity-smelling breath: This may not necessarily sound like a bad thing, but it's a sign of diabetic ketoacidosis, a potentially serious complication that’s more common in type 1 diabetes. When your body starts breaking down fat for energy, your liver produces chemicals called ketones. If too many ketones build up in the blood, they can end up poisoning the body, resulting in a medical emergency.
- Blurry vision: High blood sugar can affect the delicate blood vessels in your eyes, causing the lenses to swell and blurring your vision.
Tell me more about…
diabetes and depression
diabetes and depression
Q: I know diabetes can cause irritability, but can it make you depressed?
A: Yes. If you have diabetes, you’re at an increased risk of developing depression. People with diabetes are two to three times more likely to have depression than those without diabetes—plus, less than half of people with diabetes who have depression get diagnosed and treated. About 25% of people living with diabetes suffer from depression, compared to just 4% of the general population.
Q: Whoa—so what’s the connection?
A: It’s not fully understood. For one, the stress of living with diabetes, a condition known as diabetes distress, can certainly take a toll on mental health. But there also might be something happening on a physiological level. One study of patients with type 1 diabetes found that high blood sugar raises glutamate, a neurotransmitter associated with depression.
Q: What about the other way around?
A: There is indeed some evidence that depression increases your risk of diabetes since high levels of cortisol—the stress hormone—can lead to elevated glucose levels and increase insulin resistance. “It becomes a vicious cycle in some cases,” says Ahmed. A study in JAMA Internal Medicine found women with depression were 17% more likely to develop diabetes.
Q: Can you treat the depression by treating the diabetes and vice versa?
A: It depends. “If someone has severe depression that's making their diabetes worse, you have to treat the depression alongside diabetes,” says Ahmed. “If someone has a more mild depression that's worsening with rising blood sugar levels, then treating the glucose will typically improve mood.” And while treating depression won’t magically get rid of diabetes, research shows that taking antidepressants can improve blood sugar control.
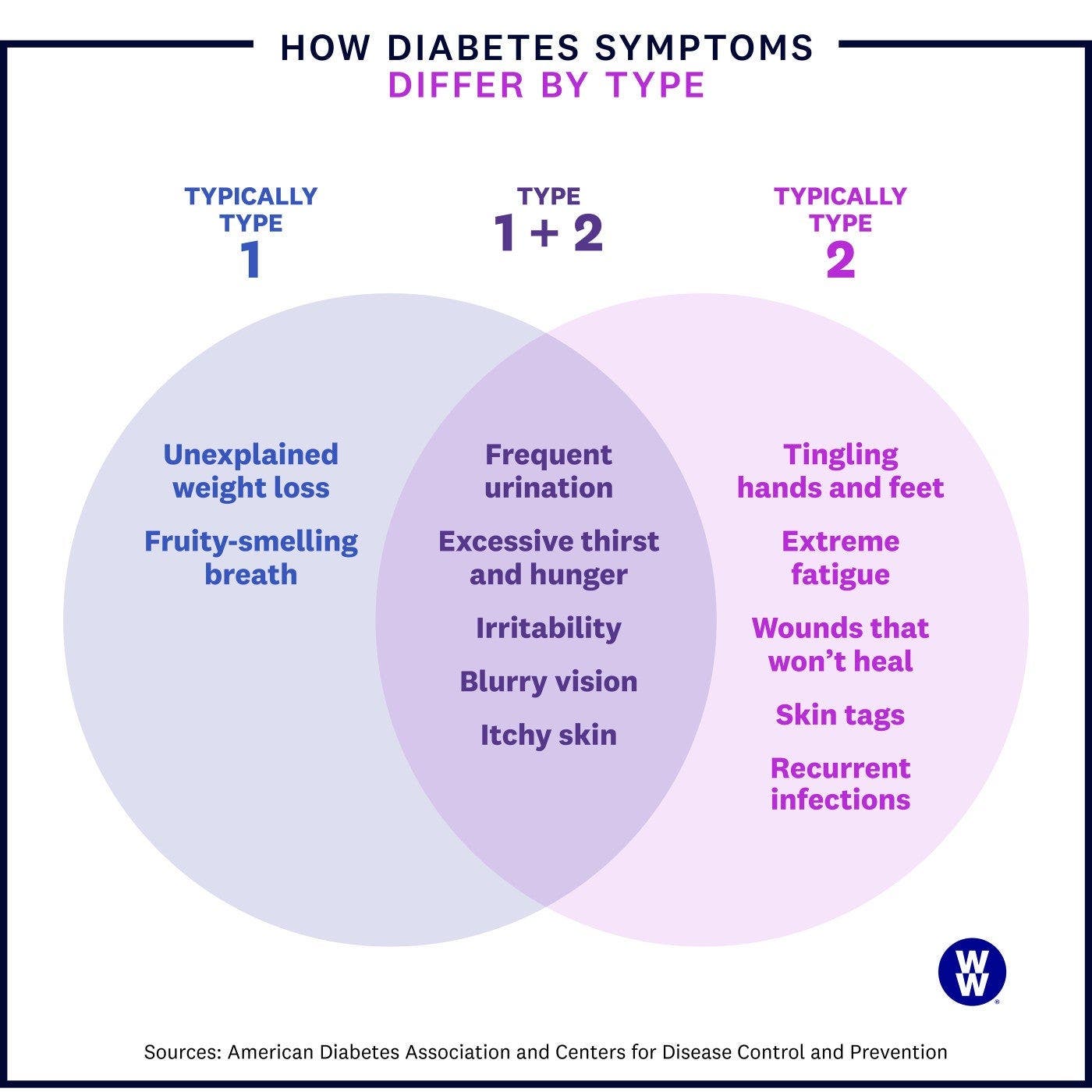
Do the symptoms differ by type?
The signs of diabetes are generally the same for type 1 and type 2, with a few exceptions.
- The symptoms of type 1 may show up more suddenly. With type 1 diabetes, your pancreas stops making enough insulin. This can cause symptoms to come on quicker compared to type 2, where insulin resistance may develop over time.
- Weight loss is more common with type 1. You lose weight with type 2, but it's more likely in type 1, since insulin may be lacking entirely for a while before you're diagnosed.
- Tingling, pain, or numbness in the hands and feet is more common with type 2. These symptoms are often a result of having undiagnosed high blood sugar for years, which is more likely to happen with type 2.
Are the symptoms different for men and women?
For the most part, diabetes symptoms are the same no matter your sex assigned at birth. But there are a few exceptions. Erectile dysfunction and impotence occur in up to 80% of men with diabetes—the blood vessels and nerves involved in an erection can get damaged from high blood sugar. This is something that likely wouldn’t happen until after you’ve had diabetes for some time, says Ahmed. Women, on the other hand, are likelier to experience recurring vaginal yeast infections. Men can get yeast infections, too, but they occur on the skin and groin. Women are also at a higher risk of diabetes-related urinary tract infections due to the anatomical structure of their urinary tracts.
So how do I know if I have diabetes?
A doctor will need to diagnose you, which can be done a few different ways.
- Fasting plasma glucose test:
Glucose levels are checked after you haven't eaten for 8 to 12 hours.
How to interpret the test
- A sugar level of 99 mg/dL or less, is considered normal.
- Between 100 mg/dL and 125 mg/dL is prediabetes.
- A level of 126 mg/dL and up is diabetes.
- Oral glucose tolerance test (OGTT):
At the start of this two-step test, you're given a very sweet liquid to drink. Two hours later, your blood is drawn to see how your body processed the sugar load.
How to interpret the test
- A blood glucose level lower than 140 mg/dL is considered normal.
- From 140 mg/dL to 199 mg/dL is prediabetes.
- A level of 200 mg/dL or higher is diabetes.
The OGTT is most commonly used to diagnose gestational diabetes, which is indicated if your blood sugar is 190 mg/dL or higher.
- HbA1c (or A1c) test:
Your doctor may also check your average HbA1c level with this test—a longer-term (over three months) measure of blood sugar control. Sugar binds to a substance called A1c in your blood, so when your sugar is elevated, your HbA1c level will be too. “HbA1c levels are important to check if you’re taking oral steroids, since they can raise the blood sugar level on a fasting blood test,” says Sassower.
How to interpret the test
- An HbA1c level under 5.7% is normal.
- A level between 5.7% and 6.4% means prediabetes.
- Anything above 6.5% means diabetes.
This content is for informational purposes only and does not constitute medical advice, diagnosis or treatment. It should not be regarded as a substitute for guidance from your healthcare provider.
