The most important things to know about unusual diabetes symptoms


What are the most unusual symptoms of diabetes?
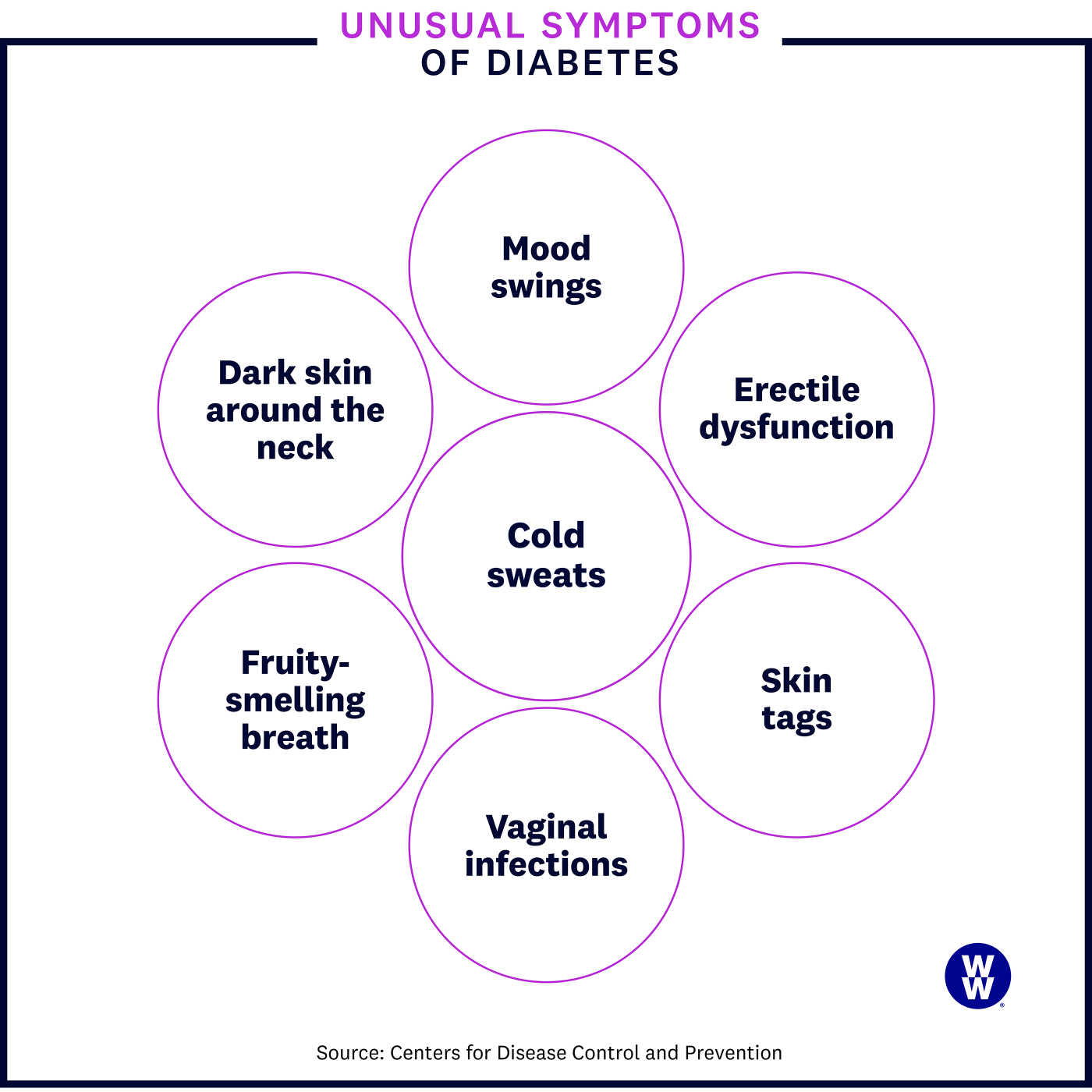
Here’s the tricky thing about spotting signs of diabetes: It’s entirely possible that you won’t experience any symptoms early on—or if you do, you may not necessarily associate them with diabetes. That’s because not all diabetes symptoms are as well publicised as, say, having to pee all the time. Some symptoms are rare. Some symptoms don’t seem at all related to diabetes. And some symptoms are just plain weird. The more unusual and unexpected signs of diabetes can include:
- Acanthosis nigricans, a darkening of the skin in specific areas of the body, like the folds at the back of the neck
- Reactive hypoglycaemia, which can make you feel shaky or weak or break out in a cold sweat, often a few hours after a carb-heavy meal
- Recurrent infections, such as urinary tract infections and yeast infections, or wounds or skin infections that take longer to heal
- Blurry or changing vision, where colours seem off or you see spots and flashes (signs of something called diabetic retinopathy)
While some of these symptoms (like a dry mouth) may be one of the first things you notice, others (like erectile dysfunction or diabetic retinopathy) are typically the result of months or years of uncontrolled blood sugar, so they won’t show up until further down the line.
Acanthosis nigricans
Acanthosis nigricans (AN) is a condition where discolourations occur on certain parts of the body. The dark areas—which can look tan or brownish across all skin types and might also be slightly raised or velvety in texture—typically show up on the armpits, elbows, groin, and, most commonly, the back of the neck.
Experts don’t know exactly why AN occurs, but they do know that it’s associated with insulin resistance (when your body doesn’t respond correctly to the insulin it makes, causing high blood sugar) and that it could be a sign of prediabetes or type 2 diabetes. If you know what to look for, AN can be a helpful sign to see a doctor: One study found that 36% of people who had just been diagnosed with type 2 diabetes had AN in their neck areas.
AN can happen to people of any age, including kids. That said, it tends to show up most often in people who are overweight, who have obesity or have metabolic disorders such as metabolic syndrome according to DermNet New Zealand and the New Zealand Dermatological Society.
The good news is that improving your insulin resistance—something that typically happens with weight loss—can help AN go away, says Dr. Amy Warriner, M.D., a Professor who specialises in endocrinology, diabetes, and metabolism at the University of Alabama, United States and the Director of the UAB Weight Loss Medicine program. Beyond that, there are no specific treatments for the condition, though a prescription gel or cream, antibiotics, or laser treatments could help. “There is limited data about using prescription creams to treat AN, so a dermatologist can provide guidance with this,” notes Dr. Ari Geliebter, M.D., Chief of Endocrinology at Holy Name Medical Center in Teaneck, New Jersey, United States.
Reactive hypoglycaemia (low blood sugar)
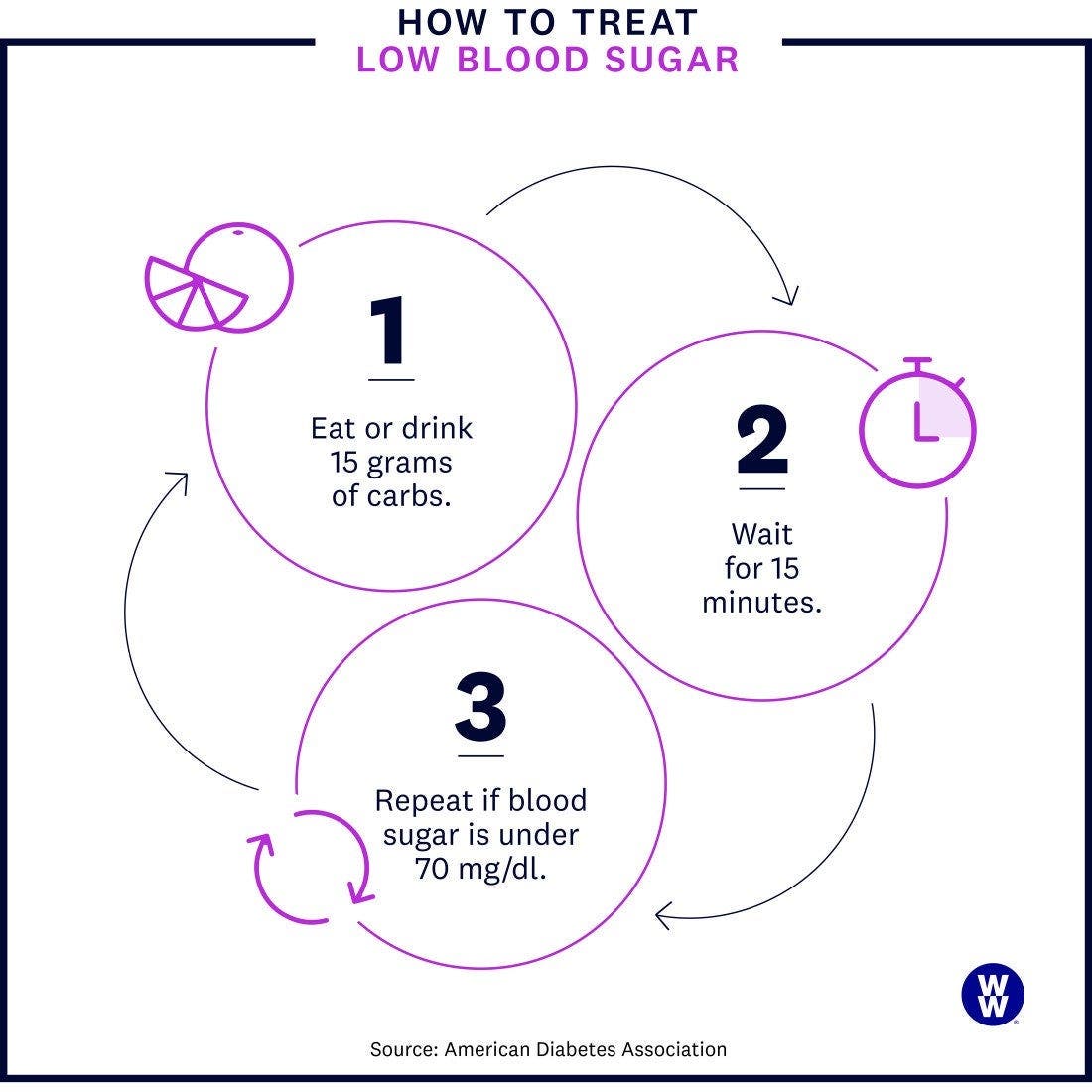
If you have a sensation of low blood sugar (feeling shaky or weak or breaking out in a cold sweat) about two to three hours after eating a carb-heavy meal, you could be experiencing reactive hypoglycaemia, also known as postprandial hypoglycaemia.
When someone with prediabetes or early type 2 diabetes eats foods that are absorbed rapidly (like refined carbs or simple sugars), their body produces too much insulin. “To oversimplify, the insulin lasts longer than the sugars that are consumed, so once the sugar is used up, the insulin is still around and active,” says Warriner. “This ultimately leads to low blood sugar.”
To relieve symptoms, try eating or drinking something naturally sweet (like an orange or half a cup of orange juice), says Warriner: “You feel better after eating again because you are providing your system with more sugar.” Reactive hypoglycaemia is also less common after meals that include lean proteins and healthy fats, so including those on your plate can be helpful.
Recurrent infections
People with poorly managed high blood sugar can be at risk of getting an infection in the same area over and over again or having an infection that takes longer to heal. There are two reasons why:
- High blood sugar impacts the immune system. Infection-fighting white blood cells don’t function as well when blood sugar is high, making it harder for you to fend off infections, as well as increasing the risk of those infections spreading, says Geliebter.
- High blood sugar fosters the growth of bacteria and fungus in certain areas. When blood sugar levels are high, excess sugar shows up in your urine, creating a great environment for bacteria and fungus to grow: “Fungus loves sugar,” says Warriner. This can lead to issues like urinary tract infections or yeast infections.
For some people, recurrent infections might be the first hint that something is up. Here are a few to keep an eye out for.
- Urinary tract infections (UTIs)
As a result of high levels of sugar in the urine, UTIs are typically marked by intense pain while peeing. UTIs are more common for people who were assigned female at birth, due to the fact that they have a shorter urethra, giving bacteria easier access to the bladder.
- Skin and soft-tissue infections
These can look like anything from an infected nail to a skin abscess (a pocket of pus that looks like a big pimple under the skin). These kinds of infections can happen in anyone, but someone with poorly managed blood sugar will notice that they take a long time to heal.
- Yeast infections
The same high levels of sugar in the urine that can bring on a UTI can trigger a yeast infection. When this happens, you may feel itching or irritation or have pain when you pee.
Tell me more about…
diabetes and yeast infections
diabetes and yeast infections
So, how chronic of an infection are we talking about?
“Recurring yeast infections would be ones that happen more than once a month in my opinion,” says Dr. Amy Warriner, M.D., an endocrinologist.
Do the usual over-the-counter treatments knock them out?
While they can help, Warriner explains that over-the-counter treatments often become less effective with recurrent yeast infections due to the development of drug resistance. That’s why you’ll want to call your doctor for a prescription if you’re dealing with recurring infections.
Can these fungal infections happen anywhere else?
“Other fungal infections are possible, including infection under skin folds—think under breasts and belly skin—but the vaginal area is more common because of the increased glucose in the urine,” Warriner says.
Erectile dysfunction
While it likely won’t be one of the first signs of diabetes, erectile dysfunction (ED) can be a longer-term side effect of uncontrolled high blood sugar. The reason: High blood sugar can negatively impact the nervous system, and when nerves are damaged, it can be tougher for a man to have an erection, according to Geliebter. People with diabetes are also often on blood pressure medication, which can have ED as a side effect, he says.
As surprising as it may be to hear that ED is a sign of diabetes, it’s incredibly common: Researchers looked at 145 studies and found that ED impacted about 52% of men with diabetes—a number that’s more than three times higher than those without the disease.
While medications such as Viagra can help, they won’t solve the problem. “The nerve issues causing the ED are hard to reverse completely,” says Geliebter, who says that, in this instance, prevention is key.
Mood swings
It’s something anyone who’s ever been hangry knows: “Some of us are really sensitive to fluctuations in blood sugar,” says Warriner. And those fluctuations can impact how we feel. Studies have found an association between feelings like anger and sadness and blood sugar levels that aren’t well regulated, but more research is needed to get a clearer picture of the glucose-mood link.
- What high blood sugar does to your mood
If your blood sugar spikes and then returns to its original level, that change could leave you feeling low, irritable, or just generally moodier than you would be if your levels were more stable. If blood sugar stays consistently high, which is known as hyperglycaemia, you may feel lethargic and tired. “It zaps your energy because it’s very stressful on the body,” says Warriner.
- What low blood sugar does to your mood
Low blood sugar, called hypoglycaemia, can result in feelings of irritability, confusion, anxiety, or nervousness. This is often coupled with physical symptoms, like sweating, headaches, or dizziness. One reason: When blood sugar levels drop, your body releases the hormone epinephrine, which can bring on feelings like anxiety. Severe hypoglycaemia can even cause you to lose consciousness and lead to other dangerous health issues.
Blurry vision
High blood sugar levels can make the lenses of your eyes swell, which, in turn, can change the shape of a lens, distorting your vision. But that scary situation usually improves quickly with diabetes treatment, often within days or weeks of getting your blood sugar under better control, notes Geliebter.
Because people are quick to notice vision issues, this symptom can be the reason people go see their doctor. “We get patients referred to us by their eye doctors who we ultimately diagnosed with diabetes,” says Geliebter.
Diabetic retinopathy
Several different eye conditions can develop over years of uncontrolled blood sugar—including diabetic retinopathy, the most widespread and serious of the bunch, according to Diabetes Australia.
With diabetic retinopathy, the blood vessels in your retinas are damaged by high blood sugar. You may notice symptoms like:
- Spots or flashes
- Colours that seem off
- Vision loss
These symptoms take a long time to come on: “Diabetic retinopathy can slowly cause vision loss and even blindness but is usually not what a patient would first notice,” says Geliebter. An eye exam can catch diabetic retinopathy, and your eye doctor will work with your healthcare team on a treatment plan, which can include medication, laser treatment, or surgery.
Dry mouth or fruity-smelling breath
One of the most common symptoms of diabetes is having to pee a lot. Your body is trying to flush out the excess blood sugar through your urine. If you’re not making up for the fluids you’re losing by adequately hydrating, you can develop a dry mouth, tongue, or throat. You may notice that it’s harder to swallow or chew your food or that your lips are cracked. As with many of the other unusual diabetes symptoms, getting your blood sugar levels under control can help.
Breath that smells or tastes fruity-like, on the other hand, could signal a dangerous condition called diabetic ketoacidosis (DKA). Diabetes Australia notes that most cases of ketoacidosis occur in people with type 1 diabetes. DKA might even be the first indication that you have type 1 diabetes.
Without enough insulin, your body can’t get the energy it needs from glucose, so it switches to using fat. This generates chemicals known as ketones—and when you wind up with too many ketones in your blood, it can be detrimental to your health.
While fruity-smelling breath is a hallmark of DKA, it’s not the only symptom. You may also have trouble breathing, your skin may be flushed, or you may have been throwing up often. If you’re experiencing these symptoms, reach out to your doctor immediately, since fast treatment for DKA is critical.
Itching and skin tags
While it’s not very common, high blood sugar can lead to dry skin and poor circulation—two things that can make you feel itchy. Diabetes can also cause skin tags, which are little growths that you might find in places like your eyelids, underarms, or thighs. Skin tags are typically caused by an overgrowth of cells on the top layers of your skin and are more frequently found in patients with obesity, insulin resistance, and diabetes, though the reason why isn’t clear, explains Geliebter.
What should you do if you notice these symptoms?
Experiencing any of the above symptoms isn’t a guarantee that you have diabetes—it’s just a sign that you might and should get checked out. “Most UTIs and blurry vision are not from diabetes, but uncontrolled sugars can cause them,” says Geliebter. “Seeing a doctor about these symptoms would allow them to assess all possible causes of the symptoms.”
The key is making sure that you’re being tested for diabetes at your annual physical check-up, especially if you’re at a higher risk of developing diabetes.
This content is for informational purposes only and does not constitute medical advice, diagnosis or treatment. It should not be regarded as a substitute for guidance from your healthcare provider.