FODMAP 101: The beginner’s guide to a low-FODMAP diet
Included in this article:
If you’ve ever eaten something that didn’t quite agree with you, you know that food can be a key trigger for a host of gastrointestinal (GI) symptoms such as bloating, abdominal pain, gas, and diarrhoea. Particularly if you’ve been diagnosed with a gut disorder such as irritable bowel syndrome (IBS) or inflammatory bowel disease, foods containing FODMAPs—carbohydrates that are poorly absorbed by the gut during digestion—could be to blame, according to the American College of Gastroenterology.
The good news? “A low-FODMAP diet may help improve meal-related symptoms,” says Dr. William Chey, MD, gastroenterologist, professor of gastroenterology and nutrition sciences, and the director of the digestive disorders nutrition behaviour health program at the University of Michigan, United States.
If you’re wondering what exactly a low FODMAP diet consists of, and if it may be right for you, read on for all the info.
What are FODMAPs?
First things first: FODMAP is an acronym for a bunch of different carbohydrates: Fermentable Oligosaccharides (fructans and galactans), Disaccharides (lactose), and Monosaccharides (fructose), and Polyols (sugar alcohols). The common thread? They're all poorly absorbed by—and rapidly fermented in—the gut. When FODMAPs reach the colon, they can become a food source for bacteria, which creates gas and natural chemicals that can cause bloating and other symptoms, according to Dr. Chey.
The four different FODMAP categories include:
- Oligosaccharides: There are two kinds of oligosaccharides: fructans (which are found in onions, garlic, artichokes, and many wheat products), and galactans (found in lentils, beans, broccoli, Brussels sprouts, and most products containing soy).
- Disaccharides: The most well known disaccharide is lactose, which occurs naturally in milk and most other dairy products like yoghurt, soft cheese, and ice cream. Typically, a naturally-occurring digestive enzyme called lactase helps the body digest lactose.
- Monosaccharides: One of the most common monosaccharides is fructose, which is found in many fruits. Because fructose is better absorbed when it’s combined with glucose (another type of sugar), fruits that have equal amounts of fructose and glucose are more easily tolerated.
Low-FODMAP foods
Foods that tend to be low in FODMAPs (but not completely devoid of them) include:
- Animal proteins: If you’re not a vegetarian, you’re in luck, says New York-based registered dietitian and nutritionist Erica Ilton, BS, who specialises in digestive diseases. Most animal proteins, including eggs, are low in FODMAPs.
- Grains: When it comes to grain products, quinoa and oats are two nutritious, low-FODMAP options, Ilton says. Gluten-free bread and cereals are also typically low in FODMAPs, according to a 2016 review of published clinical studies on IBS published in Clinical and Experimental Gastroenterology.
- Vegetables: Ilton recommends rocket, carrot, cucumber, and kale for patients avoiding FODMAPs. Bok choy, green beans, lettuce, potato, tomato, and zucchini are also good options, according to the Clinical and Experimental Gastroenterology review.
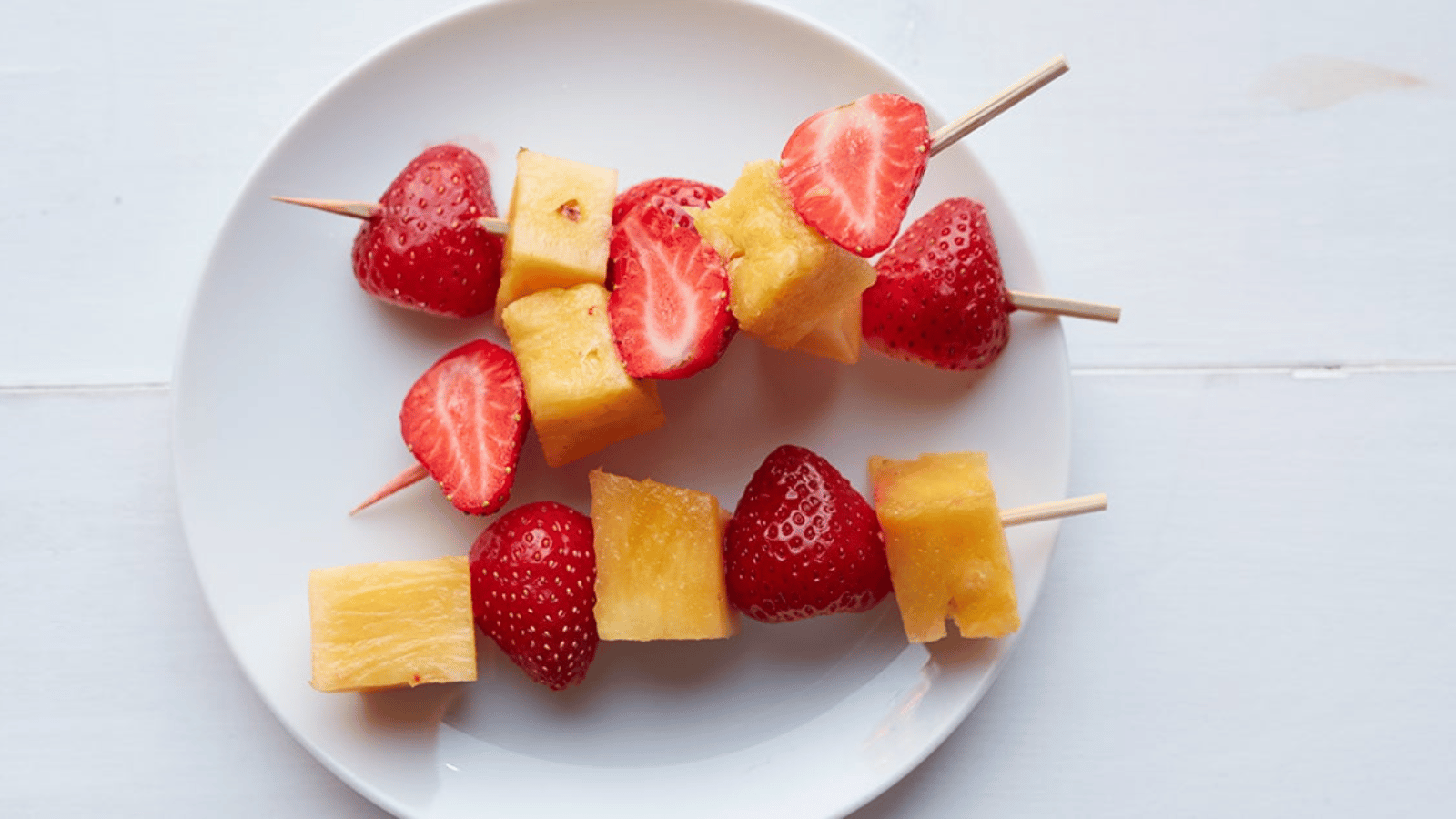
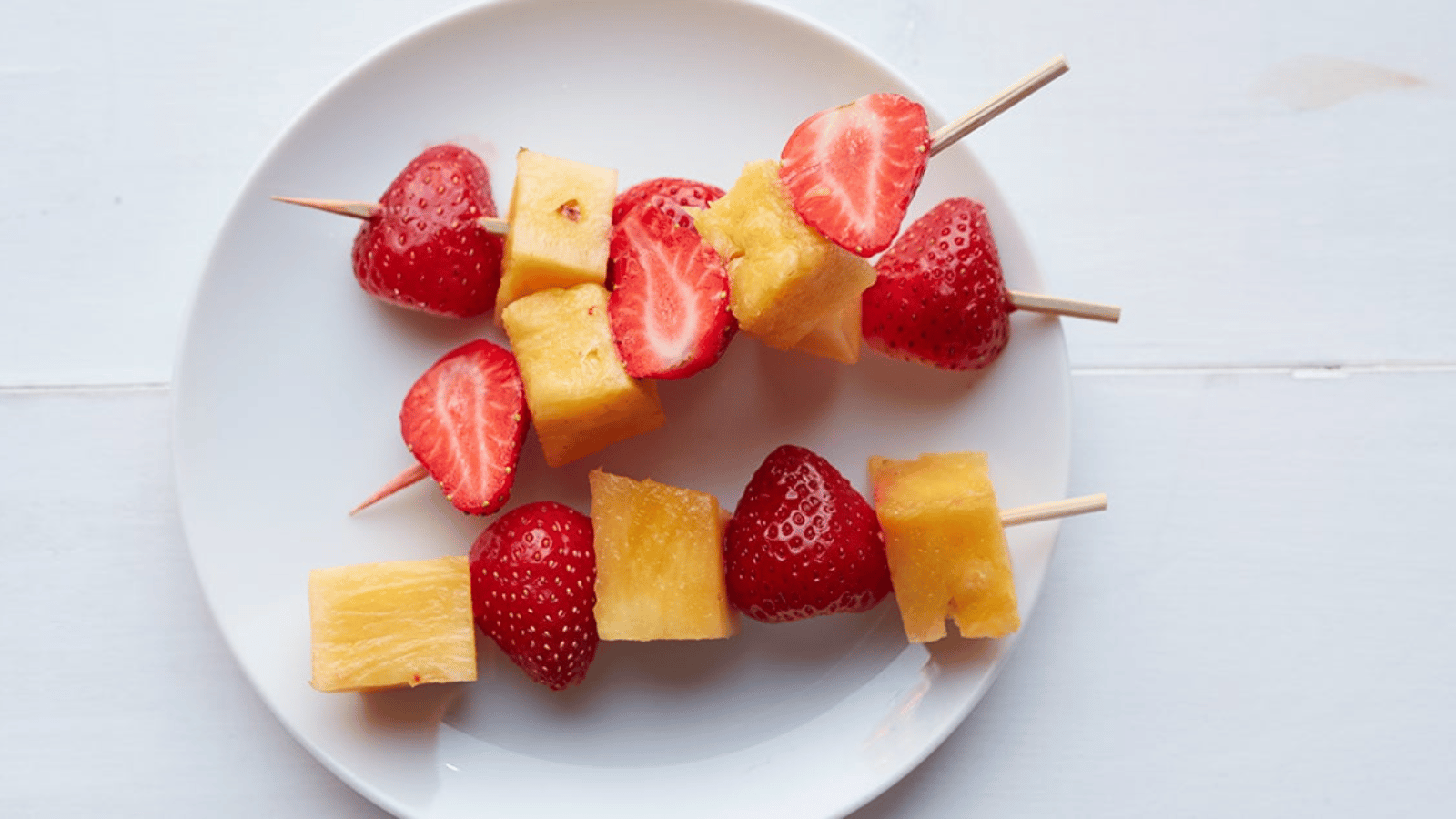
- Fruits: Looking for a sweet fix that won’t trigger symptoms? Ilton recommends oranges, papaya, and strawberries. Banana, grapes, kiwi, and pineapple are also typically safe bets.
- Dairy (and non-dairy): Hard or “ripened” cheeses (like feta or parmesan) are usually low in FODMAPs, as are almond or rice-based milk, research from the 2016 review shows.
- Natural sweeteners: Researchers from the 2016 review recommend maple syrup as a low-FODMAP sweetener.
High-FODMAP foods
While high-FODMAP foods won't necessarily trigger symptoms in everyone—everything from your genetic makeup to your microbiome, or naturally-occurring bacteria that live in the digestive tract, can play a part in food sensitivities—the bigger the serving, the more likely it is to provoke a response, Dr. Chey says. So if you’re dealing with chronic digestive issues, talk to your doctor about avoiding the following foods or eating them in small doses:
- Grains: Wheat, rye, and barley are three big offenders because they contain oligosaccharides, Ilton says, adding that gluten has nothing to do with their propensity to trigger symptoms.
- Vegetables: Found in countless recipes, onion and garlic are two very common triggers for digestive upset since they contain oligosaccharides. Asparagus, beets, and Brussels sprouts also top the list of high-FODMAP veggies, Ilton says.
- Fruits: Stone fruit like peaches and plums, as well as watermelon and most dried fruits, are high in FODMAPs, according to the Clinical and Experimental Gastroenterology review. Apples can be a big trigger too, Ilton says.
- Dairy: Regular (not lactose-free) milk and yoghurt are high in FODMAPs, Ilton says, as are fresh cheeses like cottage and ricotta.
Low*-FODMAP foods | High-FODMAP foods | |
|---|---|---|
Animal proteins | Meat, fish, pork, chicken, and egg | N/A |
Grains | Quinoa, oats, gluten-free bread and cereal | Wheat, rye, and barley |
Vegetables | Rocket, carrot, cucumber, kale, bok choy, green beans, lettuce, potato, tomato, and zucchini | Onion, garlic, asparagus, beets, and Brussels sprouts |
Fruit | Oranges, papaya, strawberries, banana, grapes, kiwi, and pineapple | Stone fruit, watermelon, apple, and dried fruit |
Dairy (non-dairy) | Hard or “ripened” cheeses (like feta or parmesan), almond milk, and rice milk | Fresh cheese (cottage and ricotta), regular milk, and regular yoghurt |
Natural sweeteners | Maple syrup | Honey, high fructose corn syrup, and sorbitol |
*These foods tend to be low in FODMAPs (but not completely devoid of them).
The FODMAP diet plan
A low-FODMAP diet restricts, then slowly reintroduces, foods that contain these badly-absorbed sugars until specific triggers are identified. It’s crucial to remember that a low-FODMAP diet is not a typical diet, it’s a diet plan, Dr. Chey says. “If you’re not going to do all three stages, you shouldn’t do it at all,” he continues, adding that the three stages should be done under the supervision of a doctor at minimum, and ideally along with a dietitian who specialises in GI issues. After all, eating a low-FODMAP diet can be restrictive, so people who try to implement it on their own may end up taking in less than the recommended daily intake of certain nutrients.
Three stages of a low-FODMAP diet:
1. Elimination
The first part of implementing a low-FODMAP diet is the elimination stage, which lasts between two and six weeks. The goal is to avoid as many high-FODMAP foods as possible, Ilton says. If there’s an improvement in symptoms, there’s a good likelihood that one or more of the foods you took out are the culprits, she continues.
2. Reintroduction
The reintroduction phase is exactly what it sounds like; systematically adding higher FODMAP foods back into your diet to see which you can, or can’t, tolerate. “I typically add one group back in at a time; the O group [oligosaccharides], the D group [disaccharides], etc.,” Ilton says.
Typically, Ilton recommends a six-day approach: During the first three days, you work with a dietitian to incrementally increase your intake of high-FODMAP foods from one category. This is followed by a three-day “washout” stage, which allows the body to properly eliminate foods that may have caused symptoms. During this washout phase, high-FODMAP foods that were previously tolerated are also avoided.
However, if someone immediately starts experiencing familiar symptoms, they are advised to stop reintroducing that group and start the three-day “washout” before testing another FODMAP group.
Because you repeat this six-day cycle for each FODMAP group, it’s not uncommon for the reintroduction part of a low-FODMAP diet to take some time to complete, Ilton says.
3. Personalisation
During this phase, you start to personalise your longer-term diet by slowly adding the higher-FODMAP foods you can tolerate back into your meals and snacks while avoiding only the foods that triggered your symptoms.
“In the end, you want someone to have as many higher-FODMAP foods in their diet as they can for enjoyment and their overall health,” Ilton says, adding that many potentially-triggering ingredients provide real health benefits.
The FODMAP diet for IBS
Irritable bowel syndrome (IBS) is a common, chronic gastrointestinal disorder that is characterised by cramping, abdominal pain, bloating, gas, diarrhoea or constipation, or both. These symptoms may increase or decrease in severity over time. IBS presents with no signs of visible damage or disease. If you believe you may have IBS, it is important to consult your doctor for a correct diagnosis.
Whilst there is no known cure, some people are able to relieve their symptoms by managing their diet, lifestyle and stress levels. More severe symptoms may require medication.
Although foods high in FODMAPs don’t necessarily cause IBS, they can stir up symptoms since they aren’t easily digested and put additional strain on the digestive tract. One line of defence against the condition, a low-FODMAP diet has been shown to have a favourable impact on bloating, abdominal pain, and diarrhoea, according to a 2017 meta-analysis of six studies performed on adults with IBS published in the journal Nutrients. However, more research is needed, especially in regard to the long-term nutritional impact.
Low-FODMAP diet recipes
While it can be difficult to find recipes during the elimination stage of a low-FODMAP diet plan, an accredited practising dietitian who specialises in gastrointestinal disorders can help you come up with some satisfying ideas. If you need a starting point, consider a few of these:
The upshot: Is the FODMAP diet safe?
If you follow the low FODMAP diet plan correctly (i.e., under the guidance of a dietitian), it can be perfectly safe, according to Dr. Chey. However, “you need to go through all three stages,” he says.
That said, experts agree that low-FODMAP diets are for specific gastrointestinal issues and should not be used as a way to lose weight. Because so many higher FODMAP foods—like garlic, apples, and beans—are nutritious, “no dietitian wants to remove them unless they absolutely cause symptoms,” Ilton says.
If you’re cutting out a lot of foods without replacement, a dietitian can help you come up with ideas to fend off hunger. At the end of the day, the best way to know whether the FODMAP diet works for you is to assess how you feel, which should be significantly better.




